Answers: How should physicians get paid?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
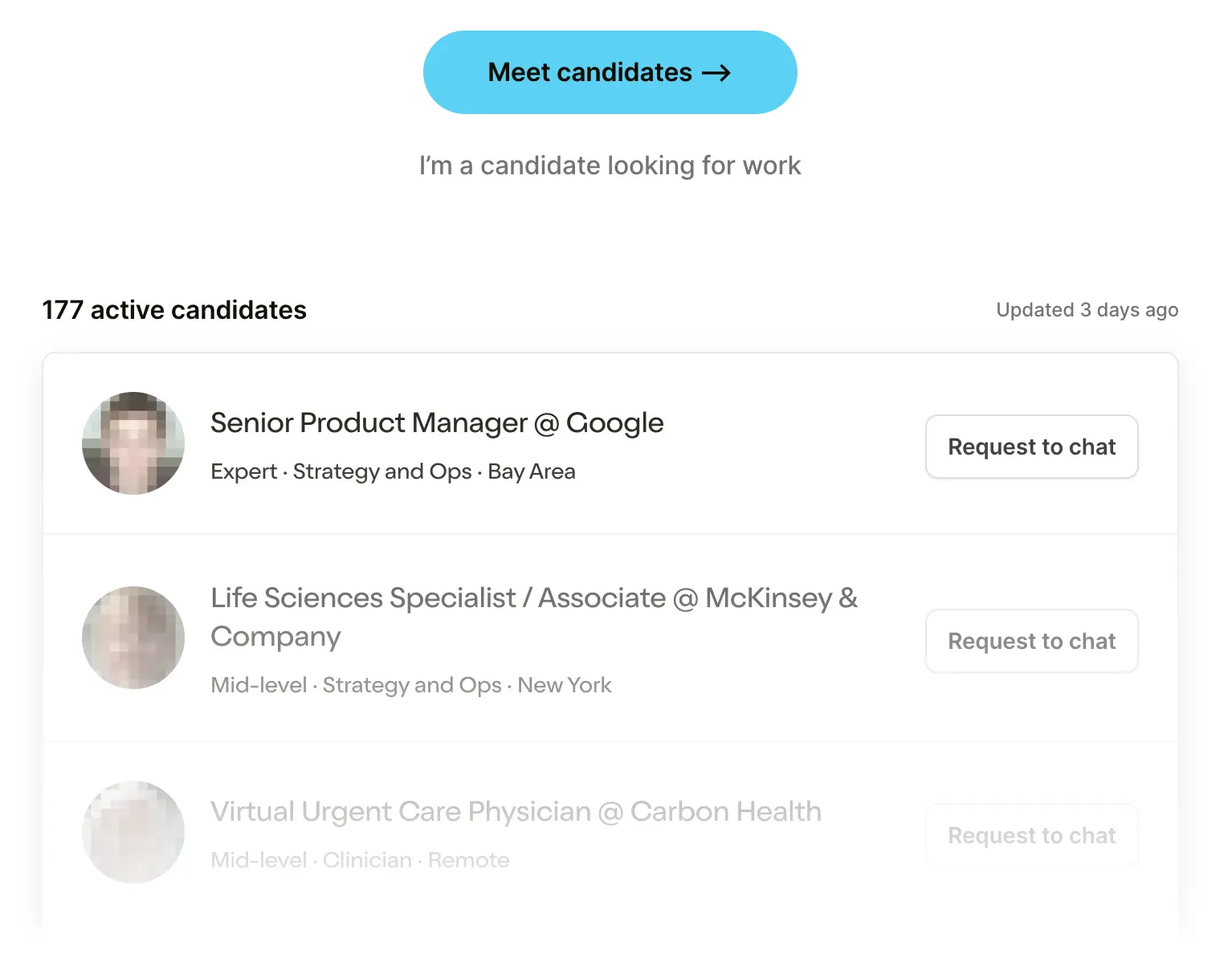 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare Product 201
.gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
A couple weeks ago I asked “how should physicians be paid?”. My general answer was that our current rules to separate physicians and financial incentives were inconsistent and put physicians at the mercy of large hospitals who get to choose the rules of compensation for physicians.
I wanted to ask what others thought about how physicians should get compensated as well. Here are some of my favorite responses.
“Eat What You Kill” - easily the worst motto for non-cannibalistic surgeons
“Without going into too much detail, I have seen what happens when surgeons in particular are in an rVU ("eat what you kill") practice. These are mostly private practice, but many hospital-employed either become rVU based/productivity after the initial 2 year guarantee. I have witnessed time and time again over decades unnecessary procedures being done. When you are passionate about what you do and love being busy and when you practice ethically with attention to outcomes and what's best for the patient, then you should be paid fairly within fair market value and not production based. This allows you to focus only on the patient and not your bank account.”
[NK note: Determination of fair market value is unfortunately the hard part :-/ I actually think ironically RVUs were created and implemented to try and created more standardized “units” to attribute fairer values between procedures, visits, etc. though correct me if I’m wrong]

Fiduciary Duty For Physicians?
“I think physicians should be held to the fiduciary standard in recommending care for their patients which is currently not the case nationally (maybe there are some state laws to this effect, but I haven't found them). See https://scholar.law.colorado.edu/.
This was recently passed for financial advisors and there's no reason it shouldn't apply to doctors as well. The only way to be a proper fiduciary is to know (a) the quality of care of another physician/practice and (b) the cost and other burdens placed on the patient in seeking care there.
Right now, every physician I've talked with is scared to death of asking other physicians what they charge for services because of the risk of being sued for price fixing. It might be possible to nullify this existing law by requiring that they confirm patient costs before referring to another physician without any exceptions for providers in the same practice or group. At the very least, this would mean a physician to physician referral price sheet which was shared among all physicians even if not with the general public. Patients in the know would be able to press their primary care doctor for the best quality / lowest cost referrals and those (underpaid) PCPs who referred a lot would gain a lot more clout among patients and specialist physicians. The only conflict of interest I can see here, especially with documented rates that are reported to the state regulators, is a physician who routinely refers to other physicians with the highest tier rates. But this is easy to spot and correct.”
-Brendan Younger
[NK note: Who is building the levels.fyi for physicians?? Also tricky because good physicians will probably charge more, so wouldn’t more physicians routinely try to refer to expensive physicians if they’re trying to get the best care for their patients?]]

Physician-Owned > Physician, Owned
“Appreciate these thoughts. I’m part of an independent Ortho practice currently in BPCI-A. We have done well in the program, but the target price is shifting downward so, like most others, we will likely drop out when the blood is squeezed from the stone. Many have argued that CMS is not giving enough credit for the extra work you speak of, and you don’t negotiate with them.
There is an undercurrent of most assuming that the majority of physicians simply overuse services and offer low value care in a fee-for-service environment. I don’t think FFS is inherently evil and certainly this happens, but we haven’t figured out the secret sauce of value-based care. I do think there is a future in physician practices direct contracting with insurance companies for disease specific bundles. In other words, I manage a patient’s hip or knee arthritis including operative and non-operative care. But there has to be transparency on both sides. Determining value is difficult. As you point out, there is the problem of cherry-picking the healthy, low-risk patients and lemon-dropping the high risk. Not good for access, but current risk stratification methods are lacking.
Physician payments aren’t the problem: Surgeon Reimbursement Unchanged as Hospital Charges and Reimbursements Increase for Total Joint Arthroplasty - PubMed (nih.gov)

There are plenty of other examples. Some physicians have side hustles or do consulting, but many don’t. In Orthopedics, we have been able to take advantage of passive sources of income through physical therapy, MRI, and DME ownership, and more recently through ASC ownership or partnerships. Physicians can also partner with hospitals through gainsharing or co-management agreements. There are lots of rules surrounding these, but the government has expressly encouraged them as a cost savings measure – they do not violate Stark Laws or anti-kickback if structured properly.
There is evidence that physician-owned hospitals provide lower cost, higher quality care, but the PPACA put the kibosh on this. Critics would say these facilities cherry pick and leave the sicker, higher risk patients for the hospitals, but we are doing more and more complex patients in the ASC setting.
I wonder if we will eventually see the pendulum swing back to physicians leaving employed positions and becoming independent. There is going to be continued downward pressure on hospital reimbursement which will translate to more work and less pay for employed docs. I hope we haven’t reached the point of no return. Private equity is a separate conversation. Is there an opportunity for a non-PE, non-hospital, non-insurer entity to partner with physicians in a more patients-over-profits approach? There would seem to be, but not sure anyone has the appetite. Would Apple, Google, Amazon want to tackle this? Would they be any better than the aforementioned entities? Some rumor that Apple tried (and failed) to open its own medical clinics.
Maybe self-serving, but I don’t think it’s necessarily wrong for physicians to be financially motivated. That doesn’t excuse gaming the system. The challenge is separating outright fraud from overutilization and “aggressive” billing and coding practices. But healthcare isn’t really a free market to help drive transparency, outcomes, and value.
Attached is my own hairbrained pipedream of how you could build a true Center of Excellence around MSK care.”
[NK note: The running theme seems to be figuring out the difference between fraud, unnecessary/low value care, and business as usual. If we were able to do that effectively and penalize properly, would we be more comfortable with physicians directly making money when they deliver care to us?
I am also betting that the pendulum swings towards more physicians going independent, and it’s a core investing thesis of mine.]
Thinkboi out,
Nikhil aka. "secure the (banana) bag"
Twitter: @nikillinit
{{sub-form}}






