Big Changes Coming
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Day 7 of quarantine:
Rearranging the furniture so it feels like I went out somewhere.
I’ve sharpied mustaches on some quarters to pretend like I’ve met people.
I’m engaging with trolls on Twitter just to feel something.

Honestly though, this entire saga has made me realized:
1) How privileged I am to have savings to weather out a storm like this. I really do feel for small business owners and people living check to check. This is a turbulent time and the lack of leadership around supporting these businesses makes it much worse. This chart from JPMorgan shows the amount of cash buffer businesses have, highlighting just how bad it is.

2) How bad it is for healthcare workers on the frontlines. Seriously, these people are fighting a war right now and are barely, if at all, equipped to do it. We should be figuring out as many ways to support the front line workers as possible. I’m scared for my friends and family that are working in hospitals, especially in New York.
3) On a positive note, I love how creative people are when it comes to interacting while in quarantine. Tech finally feels social and fun again, even if the backdrop is depressing. I’m running some virtual experiments in my other newsletter Get Real, you can check them out/sign up for them here (CROSS POSTING AUDIENCES #GROWTHHACKING).
On to a very long post cause this cabin fever got me SPAZZIN’.
Nothing was the same
COVID-19 is forcing the healthcare system to shift quickly, and lots of changes seem to be happening every day.
This pandemic has become a forcing function that quickly exposes a lot of the problems in the healthcare system at once. Because of how slow the industry is and the number of interest groups that fight to maintain the status quo, healthcare has been a boiling frog that has been unable to swiftly make changes and has been slowly descending into an increasingly shittier state.

Right now, multiple issues in the healthcare system have been exposed extremely quickly and everyone is interested in fixing them simultaneously. It’s also a time where if you’re an interest group pushing back against a law, you look like a huge asshole. So passing a lot of temporary regulations that are common sense is getting very little pushback.
This is creating a lot of temporary changes that are optimizing for speed of care. We’re seeing a lot of loosening for rules/laws that probably needed to be changed anyway. I’m curious what’s going to stick around after this.
Plus, these changes are happening across the entire globe with millions of people at once over a significant period of time. We’ll actually be able to look back at this data and figure out with large sample sizes whether or not these temporary measures improved outcomes for a given cohort (e.g. people in Medicare or people that had postponed). You could never ethically create a study like this - but since we’re forced into this situation, we can answer a lot of theoretical questions that have been asked during policy discussions using real world data.
I truly believe that this pandemic is to the healthcare system as 9/11 was for travel: an immediate macro event that changed the industry forever. Here are some of the things I (hope) are going to be permanently different. This might be a little less accessible if you don’t have industry knowledge, but I’ve tried to simplify them.
These are high level thoughts, I’ll go into the details of each in the future.
1. The rewriting of HIPAA.
What if I told you that a law written in 1996 around patient privacy and data sharing probably needs some updating? HIPAA was designed to protect patient records and give patients the authority to access and give their health data to whomever they choose. This law, however, has not kept up with the rise of cloud storage or mobile technology, and honestly has been bastardized into letting different entities hoard data.
Since it’s clear that worrying about HIPAA ramifications have made hospitals/providers wary of communicating with other physicians and use third-party tools, we should finally take this time to rewrite it.
Right now, HHS is actually letting people use non-HIPAA compliant applications like FaceTime or Skype in good faith to coordinate care. But it made a VERY SPECIAL CALL OUT ON THINGS NOT TO USE:
Under this Notice, however, Facebook Live, Twitch, TikTok, and similar video communication applications are public facing, and should not be used in the provision of telehealth by covered health care providers.
If you had bet me that in anyone at HHS even knew what TikTok was, I would have gladly given you odds. Maybe they saw this headline and realized they had to start paying attention.

2. Telemedicine hits the mainstream + expands.
This is the biggie that I think will really change after this. Several things are happening at once.
Doctors that have never tried telemedicine are being forced to use it, and many of them are actually enjoying it. Even my dad is giving it a shot, and he won’t even FaceTime ME. More patients are being introduced to telemedicine and many will end up finding it more convenient, especially for low-risk issues that don’t need a visit and management of chronic disease.
Forcing that kind of behavior change is big - getting someone to use telemedicine the first time is difficult, but then repeat usage probably increases once they see how convenient it is (don’t have data to back this up, just a hunch). We’ve already seen huge spikes in usage of Chinese telemedicine platforms + willingness to try more digital tools in the future.

Medicare is also reimbursing for telemedicine visits, and many commercial insurers are covering visits for the same rates they would normally have covered for an in-person visit. Reimbursement for telemedicine has always been extremely slow and a big barrier to adoption. I’ve heard MANY cases where doctors basically insist that patients come back in for follow ups or testing just so they can code for an in-person visit. It’s dumb.
But the most non-sensical rule of all which is FINALLY being addressed during this crisis is the fact that doctors typically have had to get licensed in every single state to see a patient in that state. I have never understood this rule - the actual practice of medicine doesn’t have that kind of variance state-by-state. This has prevented many telemedicine companies from allowing doctors to see patients in different states, which is necessary if you want to balance the supply and demand loads. Duh.

One interesting change to watch is the expansion of the types of drugs that can be prescribed via a telemedicine-only visit. You can even get controlled substances like opioids via telemedicine now (don’t get any ideas). I wonder if we’ll look back on this and discover we don’t really need face-to-face visits for most prescriptions, or if we’ll realize we missed diagnoses due to lack of an in-person visit. Time will tell on this one, but we really should track this cohort of patients closely
3. Legitimacy scoring for labs, researchers, etc.
Healthcare needs a scoring function for reputation. It’s crazy how much good and terrible information was circulating through social networks. With no reputation scoring it was impossible to figure out what was legitimate.
I’ve talked about needing this in the past for doctors, but I’m starting to think we need reputation scoring for every institution in healthcare. It doesn’t necessarily need to be a ranking of “Best”, “2nd Best”, etc. because that would be breed unnecessary competition and gamification.But we need some sort of verification system that people and institutions can receive to prove they meet at least a certain level of legitimacy so we can know to take them seriously.
Figuring out a scheme that doesn’t look like gatekeeping (a lot of people who sounded the alarm early for COVID were non-experts) but would elevate legitimate work would need to be created. Maybe Klout, for the healthcare industry, where networks of peers actually stake their reputation on others to raise both of their reputations combined with data like claims, outcomes, published research, etc. depending on their role.

4. Emergency/prior authorization by reputation.
One huge way we messed up was not allowing labs to create their own tests when this started - instead they had to get Emergency Use Authorization to do it. We should have let reputable labs (maybe using the legitimacy score above) build their own tests in tandem with the CDC - this would have sped up development and dissemination of tests.
Similarly, it’s interesting to see some states are waiving required prior authorizations during this time. For context, prior authorizations are things insurance companies/payers make doctors and pharmacists do before they’re allowed to give the really expensive medications or do expensive procedures. Doctors hate them because they feel like they have to jump through hoops just to appease the insurance companies, but insurance companies use them to make sure doctors try cheaper but cost-effective alternatives first. Unfortunately it’s a huge hassle for everyone and there are entire administrative layers built just to handle prior authorizations on both sides.

It would be cool if reputable doctors (via the legitimacy scoring?) could skip prior authorizations. I’ve heard some insurance companies potentially building products like this.
5. Bounty programs for R&D.
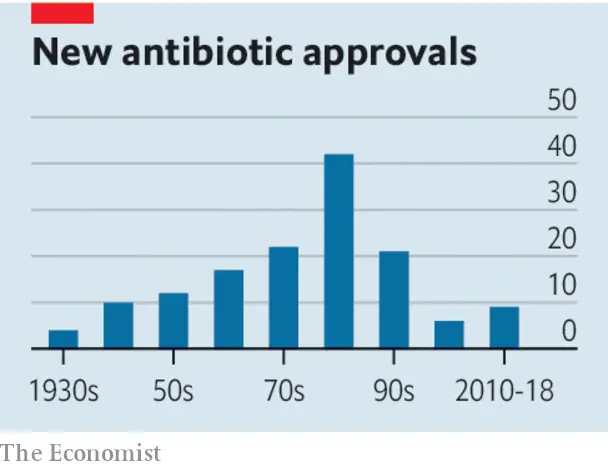
Antibiotic and vaccine development is a money pit for biopharma. To be prepared for future pandemics, we need to set up globally funded bounty programs. I talked about this in the first newsletter so won’t rehash here.
6. Aggregate public health dashboards.
Look at how sexy this Singapore public health tracker for COVID is. Most interesting part is tracking the spread by infection cluster.

In theory, we could have probably mitigated spreads if we tracked where people clustered together via GPS data from phones. China has been doing this and other countries are considering their own versions. Combined with at home diagnostics/monitoring devices could actually assess abnormalities before they even happen if that data was captured at scale.
But this also opens the door for potential misuse post-pandemic. The Patriot Act was passed for counter-terrorism measures but used in many non-terrorist use cases. It’s easy to see something like that potentially happening here too. We should really spend time thinking about the ramifications of this one for future use cases.

7. Re-evaluating number of healthcare touch points needed per disease.
With more people being forced to stay home, we might actually discover that most people actually don’t benefit from constantly interacting with the health system for their disease. In fact, we might discover that people are just as healthy with fewer therapies/surgeries for many diseases. Would be interesting to see if any guidelines change after doing a retrospective of the data (especially in conditions for the elderly, where the risk factor of each marginal intervention is not small).
Or on the flip side, we’ll see very unfortunate outcomes for patients that were forced to delay care due to COVID and will reaffirm why patients of X disease need this many touch points.

8. Redesigning anti-kickback laws
The Trump Administration was already re-evaluating anti-kickback laws, but I think that’s going to accelerate thanks to COVID. Some of the anti-kickback statutes have already been temporarily halted.
This is definitely its own post so I won’t go into all the details here, but the anti-kickback laws were passed when physicians were paid per procedure and volume of services. Examples of some things that have been considered kickbacks:
- Giving patients free equipment (like smart weight scales or smart pill bottles)
- Hospital systems giving independent physicians free software or services to better coordinate care
- Waiving the out-of-pocket costs for telemedicine services
You can see how many of these would incentivize patients to get more services, or incentivize doctors to tell patients to get more services somewhere else.
If we’re trying to move to a system that rewards giving patients high quality care, then we’re going to need to revisit these laws. Again, tricky territory and needs to be done thoughtfully, but this is good catalyst to restarting the discussions to figure out the lines between “kickback”, “coordination”, and “giving free shit for good reasons vs. bad reasons”.
If you want to give me a free scale to incentivize me into better habits you should be allowed to. I’ll just put it next to that camera I bought to get into photography and that bread maker I bought when I was sure I was gonna start baking.
9. Healthcare (infectious disease screening specifically) comes to every day areas.
One of the big changes we need to make as a society is bringing healthcare into more everyday places where people already are. My favorite example of this is a study that brought pharmacists to African-American barbershops and screened patrons for high blood pressure, which had great results. More recently, Walmart has been bringing healthcare clinics into their stores where customers are already shopping (a project I’m very bullish on). We should stop expecting patients to carve out time to go to a designated place for preventive healthcare, and start bringing some of these preventive measure where the patients are (grocery stores, their offices, etc.)
I think this is going to be a catalyst for bringing infectious disease screening into more commonplace areas at the very least. I wouldn’t be surprised if this specifically became a part of travel in the near future, considering how much of this spread was due to the amount of travel of asymptomatic patients. The new TSA pre-check is verified by sending a rectal thermometer read to them every month (which I’ve been doing voluntarily).

10. Clinical trials get serious about more remote monitoring
Similar to telemedicine, this pandemic is going to force biopharma/CROs to adopt infrastructure and tools to handle more of these trials remotely. Right now the current trials being run are at-risk and new trials will be delayed unless they can keep patients and physicians safe.
Several parts of clinical trials could probably be done remotely, but two that I think are low-hanging fruit are remote monitoring of sites and telemedicine follow ups.
Currently, clinical research associates constantly fly to each site in a clinical trial and audit them, for work that could largely be done remotely. If you masochistically enjoy both flying constantly for work and going through tons of shitty healthcare software systems, this is a job you should look into. Or BDSM.
For patients, many of the follow up visits and measurements could be captured remotely or maybe with a visit to a local lab. Administration of medicines could be done with semi-trained personnel (e.g. home nurses). Patients should still go to a clinical trial site and see the doctor regularly, but more of the visits could be pushed remotely.
The FDA has actually put out guidance for current clinical trials which makes several of these suggestions, and hopefully biopharma/CROs move to adapt some of these permanently when they see it’s just as effective (or discover it isn’t!).
- Since trial participants may not be able to come to the investigational site for protocol specified visits, sponsors should evaluate whether alternative methods for safety assessments (e.g., phone contact, virtual visit, alternative location for assessment, including local labs or imaging centers) could be implemented when necessary and feasible, and would be sufficient to assure the safety of trial participants.
- …
- If planned on-site monitoring visits are no longer possible, sponsors should consider optimizing use of central and remote monitoring programs to maintain oversight of clinical sites.
11. More startups in healthcare.
It’s been really awesome to watch people from every walk of life dive straight into healthcare to try and help. My guess is many experienced entrepreneurs and strong operators are being thrown headfirst into healthcare without ever having considered it before. They’re also bringing to the table their expertise from other industries.

I've seen many people that enter healthcare from the tech side get worn down by extremely long feedback loops + bureaucracy + regulation. Right now the loops are near instant, bureaucracy is temporarily halted, and regulations are looser. I think this will get people excited as they see their immediate impact on the industry, but might also set up false expectations if they choose to actually work in the sector long-term.
I’ve been bullish on digital health and health tech for a long time because some of the smartest people I know want to work in it now. I’m guessing we’ll see a wave of new entrepreneurs that come out of this, ready to turn their temporary fixes into actual businesses.
Or a lot of people that say “fuck this” and vow to never work in it again. And then go on to start newsletters instead.
12. Sweatpants become acceptable work clothing.
Who’s with me??? I’ll also settle for morph suits (below is a real picture of me).

If you made it to the bottom congrats! You’ve heard the ramblings of someone with mild-to-moderate cabin fever. If you enjoyed this, send it to a friend or one of the million healthcare slack groups that exist! They can sign up here.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







