Cool Facts About Health Insurance Enrollment with Aleka Gurel
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
If you missed my presentation on healthcare opportunities opening up, you can get the slides and recording here
A note: Some editions of Out-Of-Pocket going forward will be interviews with subject matter experts to learn a bit more about the nitty gritty of certain parts of healthcare. It’s a good way to learn more tactical/operational challenges healthcare companies face from actual experts in these areas instead of a hack like me. There’ll still be memes obvi.
Now that we’re deep in pumpkin spice season, which also means enrollment for individual marketplace plans has begun. If you need insurance, make sure you get it in the enrollment window!!! You can’t just sign up for it whenever you want.
To that end, today I’m interviewing Aleka Gürel. She’s a partnerships & policy manager at HealthSherpa, a company that helps people enroll in insurance.

We discuss:
- Why health insurance enrollment is so complicated
- The role of brokers
- The pros and cons of non-ACA compliant health plans
- The push back onto the exchanges and new developments with employer exchanges
- How insurers can take advantage of new technology to increase enrollment rates
1) What's your background, current role, and the latest cool healthcare project you worked on?
Aleka: In college I majored in history of medicine and ended up doing a master’s in the field, with a focus on the history of reproductive health. That led to a role at the UCSF Bixby Center, where I spent two years as a research analyst working on a study about contraceptive decision making.
I eventually decided to transition out of the academic world and joined HealthSherpa in 2018. HealthSherpa is an ACA-only enrollment platform and the largest private channel for Marketplace enrollment outside of Healthcare.gov. While most for-profit companies track their success solely in revenue, we use two metrics to judge our performance: revenue and how many people we’ve enrolled in quality health insurance. Practically speaking, that means: 1. We don't sell products like short term insurance or health sharing ministries, even though they're lucrative, because we don't consider them high-quality coverage 2. We help people enroll in every plan available on the Marketplace, even those that don't pay us a commission. 3. We help folks apply for Medicaid, even though there's no commission attached.
We’ve enrolled more than 3 million people since 2014 and accounted for about 15% of total on-exchange enrollment in the federal marketplace states last year. I currently manage our partnerships team, working with employers, nonprofits, and other folks who want to help their communities find quality coverage through the federal and state exchanges.
Last fall we launched a new mobile-friendly Medicaid flow, which allows you to submit an application for Medicaid directly on HealthSherpa.com in the 36 states that use the Federal marketplace. That’s been a really exciting and impactful project, especially in light of layoffs and closures due to COVID19, when many, many people now qualify for Medicaid based on their monthly income. We’ve already helped more than 16,000 people apply and the number of monthly applicants has tripled since March.
2) I tried figuring out how to buy insurance on the exchange and...it was literally impossible to figure out. For a marketplace for a consumer product, why is it so complicated for the user to understand?
Aleka: Insurance is incredibly complicated, and most folks have that complexity abstracted away from them by relative lack of options. If you get health insurance through your job like most Americans do, you’re choosing between maybe two plans, and that choice is a little more obvious. Maybe one’s an HMO and one’s a PPO, or one is cheaper with a really high deductible and one is more expensive but with a deductible you can afford if something were to happen. There are a limited number of questions you need to answer to make that choice.
On the Marketplace, there are often dozens of plans available to you that all look pretty similar, and it can be really hard to tell the difference, even if you have good insurance literacy. What’s the total cost to me going to be? Which doctors are going to be in-network? Which plan is going to cover my prescriptions? Two plans might have identical deductibles, but one might cover some non-preventive care before you hit that and one might not. As a consumer, especially one who doesn’t use a whole lot of healthcare, you often don’t even know the right questions to ask.
When you add subsidies and cost-sharing reductions on top of that, and factor in that if you just google “Obamacare plans,” most of the ads are going to be for sites that sell junk health insurance, it’s overwhelming. Many people don’t realize that “Obamacare”, Marketplace insurance, and ACA insurance all refer to the same thing, and that a lot of non-”Obamacare” insurance sold online doesn’t cover nearly as much health care. That’s why it’s so critical to have access to trusted enrollment counselors, like navigators, certified application counselors and brokers.
3) What's the deal with brokers? Should you enroll through them? Are there pros/cons through going with them?
Aleka: Practically speaking, brokers account for about half of all Marketplace enrollments, so most people who get a hand in enrolling are going through a broker. They are experts in health coverage and often very familiar with the ins and outs of local coverage networks, benefits of particular plans etc. Most are responsible people who have their clients’ best interests at heart and are going to provide really high quality support.
However, commissions for ACA products vary really widely, and if you’re in an area where commissions are thin or non-existent, it’s hard to make a living selling ACA plans. Coverage options like short-term, health sharing ministries, and indemnity plans don’t have to meet the same medical loss ratio standards as ACA plans - they sometimes don’t even legally have to pay out claims. That means those plans have lots of cash with which to pay hefty commissions. So there’s definitely an economic incentive for shadier folks to push people towards plans that don’t offer the same consumer protections. (And in the same vein, companies who sell these junk products can afford to pay more for keywords like “Obamacare” on Google ads, which means that folks who search for Marketplace plans often get redirected to non-ACA coverage options.)

At HealthSherpa we are a broker, but we’re a little unique in that we offer every plan available on the Marketplace without factoring in whether that carrier is going to pay us a commission or not. Commissions never play into the recommendations we make, either.
When somebody visits our site or calls one of our advocates, our first step is to figure out if they qualify for subsidies or for Medicaid or CHIP. Based on eligibility and what they tell us about how much healthcare they use and which doctors and prescriptions they need covered, we crunch the numbers and surface the plan that’s going to be the most affordable for them. And most importantly, that recommendation is always going to be for Medicaid, Medicare or a Marketplace plan that covers pre-existing conditions and essential health benefits and free preventive care.
That is, in our opinion, just the right thing to do, but it also creates an enormous amount of trust with our partners. When you work with us, you’re not going to get a situation where somebody sold your part-time employee a short-term plan that didn’t cover their cancer treatment -- or more saliently right now, their COVID-19 test or treatment.
4) So I'm sure right now during COVID there's a mad rush to get on the exchanges. What are some of the unexpected challenges that have come up in the last few months when it comes to enrolling customers?
Aleka: Interestingly, the big influx we’ve seen at HealthSherpa has been among folks eligible for Medicaid - the number of monthly Medicaid applications we process has gone up 3x, whereas Marketplace applications are up only about 20%. That makes intuitive sense, because unlike Marketplace subsidies -- which are based on your expected annual income -- Medicaid eligibility is based on current monthly income, and many people are experiencing sudden income losses.
Medicaid also doesn’t require a qualifying life event to enroll. That’s a major benefit in our current situation where many people losing their jobs are part-time and were never offered employer health coverage in the first place. These folks usually don’t have qualifying life events to enroll in a Marketplace plan - unless they’re in a state that created a Special Enrollment Period specifically in response to the pandemic.
There are however, many people out there who would qualify to enroll in Marketplace coverage and just haven’t, and there are a variety of reasons why. We’ve seen that for most people, getting signed up for unemployment benefits is understandably their top priority. Given the nationwide delays affecting that process, we suspect many people just haven’t moved on to the next task of applying for Marketplace coverage.
Many people also don’t realize that the Marketplace is even an option, especially if they’ve had employer coverage all their lives and haven’t had to rely on it before. You get your COBRA notice in the mail, see the $600 price tag, and immediately discount the possibility of getting covered, even though you likely could qualify for something much, much more affordable on the Marketplace (HealthSherpa users pay an average of $48/month). We work with individual employers to do outreach to terminating employees around this, but a much larger national awareness campaign is needed.
Even if you do get your foot in the door and start the application process, figuring out your income can be really tricky, especially if your unemployment application hasn’t been processed yet. Plus, if you qualified for the $600/week enhanced unemployment benefit, that counted towards your annual income for determining your subsidy eligibility, but not when determining eligibility for Medicaid. Our general goal is to abstract all of that complexity away from the end consumer and only ask questions they know the answer to, but that’s hard to do when people are facing so many unknowns.

5) There have been pushes in different forms for employers to get their employees to use exchanges. That can take the form of private exchanges, now we're seeing this with ICHRA plans. What are some of the pros and cons to these employer/exchange relationships and obstacles to them being widespread?
Aleka: We’re keeping a very close eye on the new ICHRAs at HealthSherpa and think there’s a ton of potential there. The current downside to the model -- where employers give you dollars in an HRA to buy your own coverage on the exchange -- is that Marketplace plans tend to have more narrow provider networks and lack some of the bells & whistles that group plans offer. However, if ICHRAs become widely adopted, carriers will respond by offering more group-like individual plans in response. In fact, certain carriers are already experimenting with more ICHRA-focused plans for the upcoming Open Enrollment Period.
There are significant benefits to the ICHRA model to employers in terms of lowering the barrier to entry to offering a health benefit, controlling health spending, reducing administrative burden on the benefits team and managing the risk of high claims. But I think one of the most compelling things about ICHRAs for employees is that it makes health coverage more portable between jobs.
If for example, you’re a full time employee offered an ICHRA by your employer, and then you work fewer than 30 hours in the next assessment period -- or, say, a global pandemic hits and you’re laid off - you can keep that same plan and likely qualify for a subsidy to replace the amount your employer was previously paying towards the premium.
When you look at reasons people list for going uninsured, changes in status - like losing a job or turning 26 - are really high up there. So anything you can do to sever the relationship between employment and health coverage is, in my opinion, a step in the right direction.
[Nikhil’s note: 26 was a bad birthday]

That said, going from being offered one or two plans to being able to choose between 70 is going to be a huge change for employees, and they’re going to need support. I think the employer “private exchange” model is going to become really important in this environment to provide employees with hand holding through the process and help them understand whether their ICHRA is affordable, whether they’re eligible for Medicaid, that they need to go off-exchange to use their cafeteria plan, etc.
At HealthSherpa we’re building out a comprehensive set of ICHRA support tools for employers and employees, and I think the unbiased consumer support model we’ve built up through supporting non-benefits-eligible employees is going to be really important. If you’re entrusting your employees to an enrollment partner, you want an advocate on the other end of the line, not an agent who’s going to push you to the most lucrative plan or upsell you. (And in fact, endorsing specific issuers or plans is prohibited under the ICHRA regulations, so you avoid a compliance headache by working with a partner who offers all available plans on equal footing.)
6) I know that insurers have generally flip flopped around having plans on the exchanges, and it's usually based on the perceived risk pool of people buying plans. Has this stabilized? Will this positive sentiment around the exchanges stay after COVID is over and people move back to employer based plans?
Aleka: The individual market has gone through a major recovery in recent years. The number of single-issuer and bare counties has gone down, premiums have stabilized or fallen, issuers are expanding into new states, and we’ve also seen some major issuers returning to the market - for example, UnitedHealthcare plans to come back to Tennessee and Maryland this fall.
Broker commissions are also a great indicator of the health of the Marketplace. A while back many issuers stopped paying commissions at all during the Special Enrollment Period, because people who enroll outside of Open Enrollment tend to be sicker and more expensive to take care of. Those commissions have started to return in recent years, which is another really positive sign.
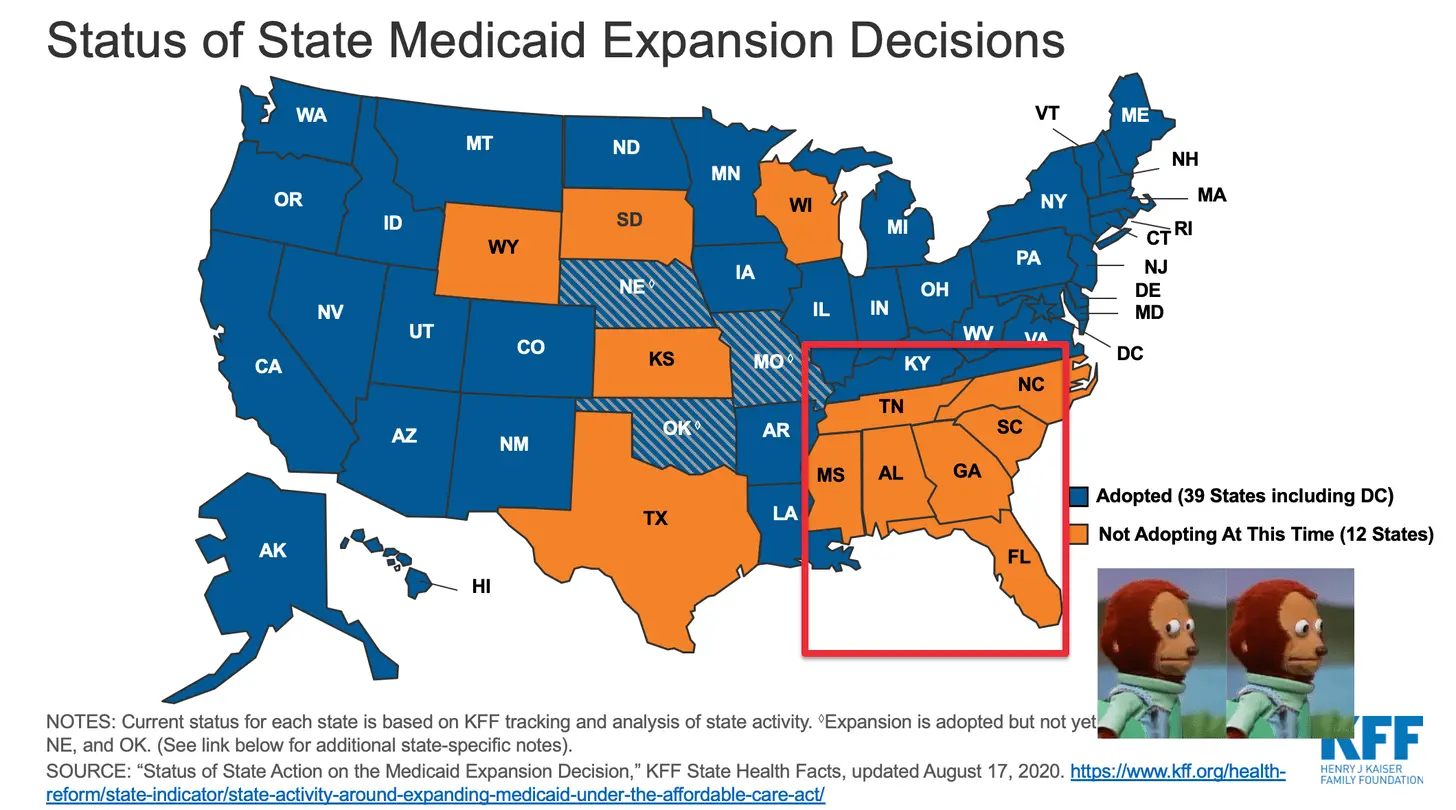
In terms of what will happen post-COVID, that depends on so many factors. I think there’s a good chance COVID will accelerate the recent trend we’ve seen towards Medicaid Expansion in states that originally chose not to cover all low-income adults. That movement is, first and foremost, hugely important for making sure our most vulnerable citizens have access to quality health coverage. However, there’s also some evidence that this has a positive impact on the health of the individual market by moving sicker, higher-cost individuals out of that risk pool and into Medicaid.
I think the question of whether everyone will, in fact, return to traditional employer based coverage after COVID is an open one. COVID has definitely accelerated interest in ICHRAs and if the CMS-DOL-Treasury predictions play out and another 11 million relatively healthy people join the Marketplace, that’s going to have a huge positive impact on the risk pool.
7) I've had friends ask me about health-sharing ministries, short-term plans, etc. What are these, who are they good for, and if you're considering them what should you look for in the fine print?

Aleka: Put simply, these are plans that don’t have all the same consumer protections as ACA plans, like covering pre-existing conditions and essential services like preventive care, prescription drugs, maternity benefits and mental health, to name just a few. Unlike ACA plans, which have an out of pocket maximum that you pay before the insurance covers the rest, these plans often put a limit on what they will contribute to your care, leaving you on the hook for the rest of the bill.
A $50,000 annual limit sounds like a lot until you get cancer or have a major surgery, which will often eat through that entire amount. In the case of health sharing ministries, they’re not even legally classified as insurance, which means you sometimes have no recourse if they just refuse to pay your bills.

Some people argue that because quality health insurance is so expensive, you should have the option to go pick something that’s not as good in order to save money. That is, in my opinion, a flawed argument for two reasons.
Firstly, many people who buy these policies would qualify for generous subsidies on the ACA exchanges and they just haven’t checked, or a shady broker never told them they qualified.
Secondly, consumers fundamentally don’t understand how much financial risk these products put them at or how they’re different from ACA insurance. Because these products are very lucrative to sell, there are many folks out there pushing them without really educating the consumer.
So to your friends I’d say: don’t consider them! Or at least, make sure you’ve truly exhausted your options and read the fine print very, very carefully. Then accept that this is a gamble, and not a “affordable alternative” to a real health insurance plan.
8) For insurers thinking about selling on the exchanges, any tips on what they can do to be successful?
Aleka: My big tip is: get Enhanced Direct Enrollment!
Back in 2018, CMS started allowing private entities to integrate directly with Healthcare.gov via a program called Enhanced Direct Enrollment (EDE), which has fundamentally changed the economics of the ACA for insurance companies who use it.
Before EDE, there was a system called “double redirect”, where you went through the plan quoting and shopping process on the insurance company’s page, then “redirected” to Healthcare.gov to fill out the application, then came back to the original website to confirm enrollment. And you also had to make a Healthcare.gov account to get most of the application follow-ups done. As you can imagine, this led to a ton of dropoff, confused consumers, and generally terrible user experience.

With EDE, the whole enrollment takes place on the insurance company’s page. That’s a huge boon for conversion, and it also makes the application a lot faster. You can also handle all your post-enrollment tasks through the carrier directly - things like getting your tax forms, paying premiums, uploading eligibility documents, and updating your application if your circumstances change. You don’t have to go to Healthcare.gov at any point - you stay in the issuer’s “walled garden.”
Another really neat feature of this is that if a particular consumer has enrolled in an ACA plan before, EDE allows you to retrieve that old application. So instead of having to start from scratch every year, the consumer can just update their old application, even if they didn’t apply with that particular EDE entity before. As you can imagine, that really speeds up the renewal process.
EDE also creates this really interesting dynamic where insurance companies find it worthwhile to directly market their ACA plans. As an issuer, you can run ads directly to your enrollment site, which only shows your plans, and it converts at a far higher rate than previous iterations. That means it’s worth it for insurers to actually spend money advertising the ACA, which is good for everybody!
HealthSherpa was actually the first entity approved for EDE back in 2018, and we account for about 90% of all enrollments going through the program. Part of the reason we’ve been so dominant is due to our singular focus on the ACA - approved entities can build unique tools on top of the core EDE APIs, and we’ve put a huge amount of energy into building functionality that further improves the UI, plus conversion and retention of consumers. That has benefited not only our work with consumers, but also the 20+ issuers who license our technology for their own ACA business.
Bonus: you have a newsletter about your cooking escapades and you recently talked about the exploration of deep frying. What tastes surprisingly good or bad fried?
Aleka: My absolute favorite thing to deep fry is cauliflower! Joshua McFadden has a wonderful cookbook called Six Seasons that’s all about celebrating seasonal produce, and there’s a recipe in it for cauliflower with a spicy fish sauce dressing. You deep fry the cauliflower just as is - no batter or anything! - until it looks worryingly burnt. Then you toss it with the spicy dressing and garlic and a little olive oil. It is wildly good.

Thinkboi out,
Nikhil aka. “you don’t realize how expensive health insurance is until you leave your job sigh”
Twitter: @nikillinit
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







