Healthcare Ideas That Look Good But Are Bad
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
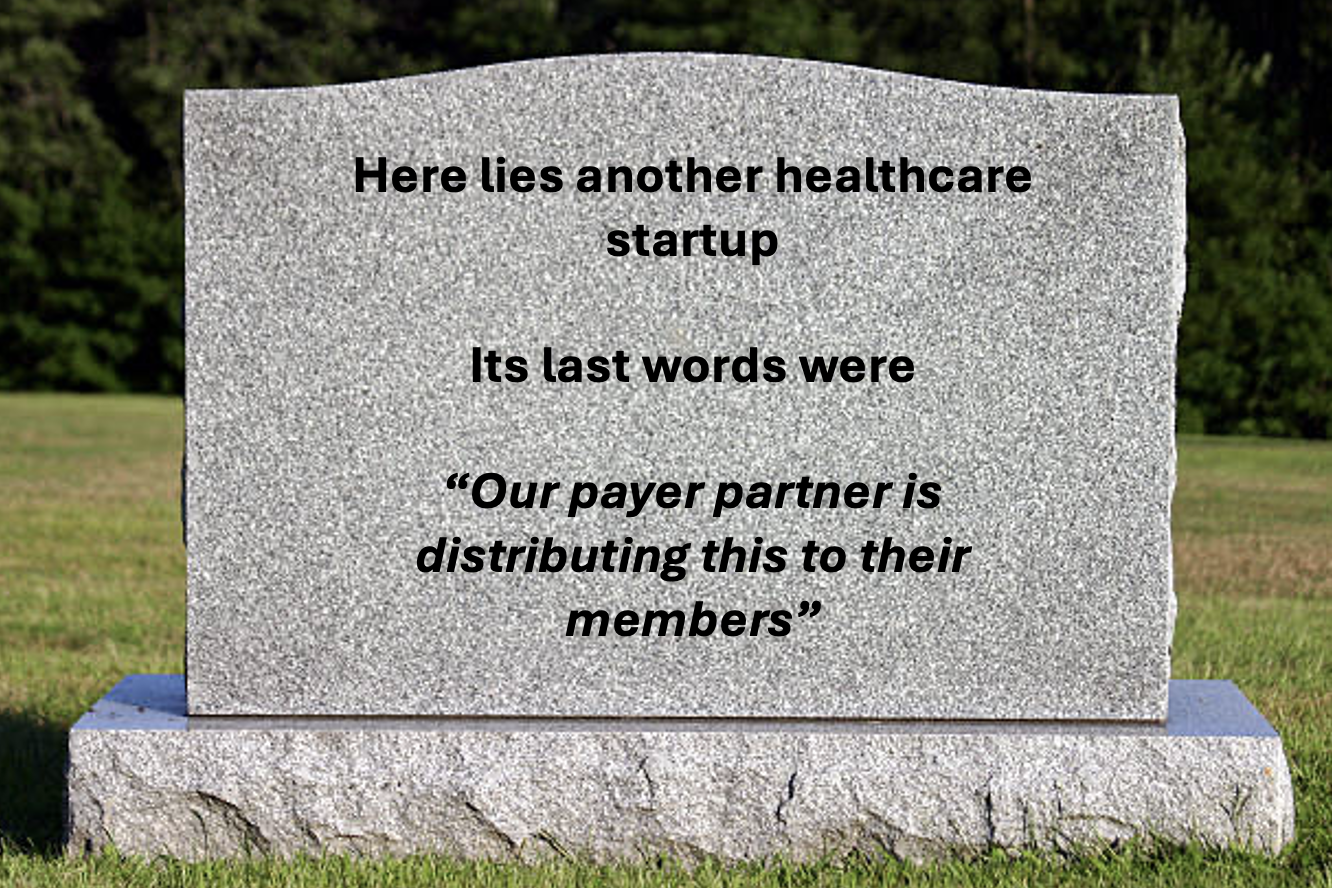
Previously, I wrote about why medical tourism was a tarpit idea that everyone tries and finds out it doesn’t work.Then I asked you all to send me other examples of tarpit ideas you’ve seen and you didn’t disappoint. Below are a few of my favorites:
- Clinical Trial Matching
- Looker for EHRs/Super App for Healthcare
- Health Insurance for Startups
- Smart Pill Bottles
- “Find a specialist”
I added some memes and commentary on each. If you or a friend are thinking about these ideas, I would read these to understand why previous iterations haven’t worked.
But before we get into the good stuff, 2 courses are ending enrollment soon.
- US Healthcare 101 Crash Course - Taught by yours truly. You’ll learn in 3 weeks what took me 8 years to figure out about how the US healthcare system works. ENROLLMENT ENDS THIS WEEK!
- How To Sell To Health Systems - This course gives you a playbook, templates, and 1-1 guidance on how to refine your pitch so it lands with hospitals. ENROLLMENT ENDS THIS WEEK!
Email nikhil@outofpocket.health for group discounts - we’ll teach your people. See the other courses here.

On to the ideas.
Clinical Trial Matching
"Clinical trial matching is textbook tarpit. But the market is SO big? Biopharma spending each year is ginormous? The problem is so glaring?!
Take your pick of dire, unicorn-in-the-making stat and you think bingo! I’m going to revolutionize clinical research by fixing clinical trial matching:
- 9 of 10 trials ultimately double their original timeline in order to meet enrollment goals
- 11% of research sites fail to enroll even a single patient
- As high as 30% of patients in US clinical trials drop out before completion
- Delayed and aborted studies costing over $100B every year
- In the United States, more than 80% of clinical trials fail to achieve targeted patient enrollment, and 30% of study participants discontinue participation.

The trap! The problem isn’t really the matching of patients to trials. It seems like it is, but it isn’t: Trust me, Martin Naley and I built some extremely good matching software a few years back that told cancer patients all the trials they are eligible for but that matching report didn’t solve the avalanche of real problems that will muck you up in the tarpit:
- There is SO much misinformation about research, clinical trials and what participating even means. There is a lot of education necessary to even get most patients to consider a trial which is “experimental” where they don’t want to be a “guinea pig” or take a “sugar pill”. Layer on systemic mistrust amongst underrepresented groups (Tuskegee wasn’t that long ago…) and turns out most patients aren’t interested in participating in research, or at least super hesitant.
- Doctors (and the health systems they are located in) aren’t incentivized to refer patients to clinical trials unless the study happens to have a trial site at your hospital (yeah, unlikely) – firstly, it’s creating more work and more complexity for them on top of typically overloaded patient loads. They just don’t have the time unless they are the rare true above and beyond ones. But structurally, they don’t have time. Time/complexity aside a referred patient to a trial = lost revenue. And if we’re talking oncology or cardiology, these are the highest clinical revenue generating patients. So probably no surprise most trials are oncology or cardiology… referring out patients means you’re losing creme of the crop revenue generating patients.
- Doctors control treatment decisions. Sure patients can come in empowered with a list of trials but at the end of the day that doctor is the ultimate decider, and most patients end up listening to their doctor and not really questioning their recommendation. Hi paternalistic medicine, is that you?
Let’s say you make it this far. You’ve got a willing patient, a trial they are eligible for and a saint of a doctor – welcome to the last mile! The tar here is THICK.
- Chances are no one answers the research coordinator email address on the ClinicalTrials.gov listing because it turns out that research assistant left that job 9 months ago. Keeping contact data up to date is spotty and poorly done, so is the status of the trial. Chances are the trial’s been discontinued or might be fully enrolled.
- The patient will likely have to travel to the research site for additional screening and eligibility confirmation, then relocate or be willing to travel (usually on their dime) in order to participate in a research study that is unpaid. Most people just can’t swing the financial burden and practical reality of travel.
And the last kicker is that clinical treatment decisions, especially in urgent conditions like cancer are made within a few weeks at most. Which means “catching” the patient and enrolling them in a study has to be CRAZY FAST. Layer on all the challenges above and the realities of the last mile and… good luck.

Despite this tarpit reality check, I remain committed to improving research, making it easier for patients to participate in research and advocating in my personal and professional lives to keep chipping away at this problem. We all need to take off the rose-colored glasses and start tackling the realities of research participation one snarled incentive and inefficiency at a time."
[NK note: People are obsessed with trial matching as the problem because it seems like a data and awareness problem when it’s really a priorities and cultural problem.
One part not mentioned is that trials also frequently are looking for a very very specific “type” of patient, which they find through inclusion and exclusion criteria. This has been getting narrower and narrower over time as pharma companies look for subgroups have as many other variables controlled for as possible. But this can eliminate a ton of patients - for example trials might look for patients that have never tried a biologic for their disease when in the US that’s usually the first treatment your doctor tries.
We talk about all the stuff that happens during a clinical trial in the healthcare 101 course.]

Looker for EHRs + super app for member navigation
"tl;dr: don’t try to build a new EMR (it can be done, but you’ll probably regret it), a tech-enabled insurance company is just an insurance company, and yes, we know, finding a doctor is really hard. It’s not a secret. Let’s explore the first and third in more detail.
One idea that I’ve seen dozens of times over the years is the modern EHR pitch. It sounds good in theory, right? EHRs are (mostly) terrible pieces of software to work in, have 90s UX/UI, don’t hold structured data, and were designed initially for billing. Providers spend countless hours clicking in an EMR and burnout is at an all time high. But, at the end of the day, a better interface is a nice-to-have and replacing whatever’s already there is a massively uphill battle. In theory, it could lead to better quality outcomes (but that’s hard to prove), and in our FFS-centric environment, it doesn’t facilitate higher billing rates or increase patient volume. What folks often forget is that the overall provider SaaS market is limited and selling into the space is a long road. Even Epic, the market leader and arguably the most critical tech player in provider IT, only brings in $4B+ of revenue a year according to Forbes. Is that really something to chase?
The pitch I actually heard more often was that "I'm not building a new EHR, just a Looker-like interface for docs. Something to sit on top of the EHR to make it useful and enjoyable". It's often the same story: an entrepreneurial doc builds a custom specialty-specific visualization tool for its providers to use in one of its hospital departments. They want to spin it out and raise venture funding. But, it never even leaves the 4 walls of the hospital because it’s too complicated to build out custom workflows for every specialty, no one can agree on what they want to see on the core screen, and few providers want to sit for hours customizing their screens. Even if it did spin out, thinking through all those integrations makes me 🤯.
Another idea that I’ve seen countless times over the years is the super app for care or member navigation services. It comes in many shapes and sizes (help us find you the best doctor, come to us first and we’ll triage you, we’ll build a better provider directory, we’ll show you pricing and let you choose better, etc.). Anyone remember Jiff?
Arguably, marketplaces around care have worked in subspecialties, like mental health or urgent care, but why is it so hard to build a tool that helps with everyday navigation? There’s definitely consumer demand - just take a look at how many people search for “find a doctor near me”. First we need to start with who pays? We’ve seen tons of low PMPM employer plays, but it turns out that members rarely use it, and the value ends up being driven entirely by steering to lower intervention providers. So, unless you're dealing with surgeries, you're out of luck. Plus, it’s super hard to be top of mind when a care need hits, and most health apps just aren’t “magical” enough to really break through the noise or warrant a monthly consumer subscription.

What both of these have in common is the ability for AI to make both of these spaces much more interesting by moving closer to the care transaction. If we zoom out, maybe some of the dictation and AI scribe companies start to look a bit like EHRs down the road. Their utility was not possible in a pre-LLM world, and I’m excited by some of the clinical decision support functionality that I’m seeing out there today. The EHR is just a way to document what’s happening between the patient and the provider. What if that interface disappears entirely because patient services are delivered entirely by an AI agent. After all, if you look at historical healthcare spend, value has always accrued to the entity delivering the care, not the software sitting in the middle. Maybe these care navigations services don’t just match you to the care but provide it themselves. We’ve all followed the Babylon saga (once valued at 2B, filed for bankruptcy), but what if they were just too early?"
[NK note: There’s an entire class of startups that have not worked previously that actually might work thanks to AI because
- Custom software development costs come down dramatically
- Some form of labor costs that’s usually prohibitive drops dramatically (e.g. phone calls to verify some information)
- You can build totally new interfaces that can map to the right places in the background without needing to totally rip out legacy tech]
Health insurance for startups
"Disclosure: I learned this from experience. The idea of building a health insurance plan targeted at startup businesses seems like a great idea for many reasons.
- Startups are underserved by the existing market where they overpay for health insurance for their employees
- Startups are young and healthy, so you likely don't need to be very good at things like case management to start.
- Startups want a "self-signup" process that feels very easy to build.
- It's possible to distribute to them efficiently through VC relationships and Hacker News posts.
- You don't have to sell through a conservative HR layer, the benefits buyer is a real human who believes in startups.

The idea is actually a bad one.
- Buyers know so little about health benefits that they are extra risk-averse when selecting insurance
- There are regulatory barriers to offering self-funded plans in most of the states that have a high concentration of startups. PEOs have managed to exploit a few loopholes that let them operate, but the door is closed to others.
- Despite startup people being young and healthy, they are actually very high-maintenance and have higher and weirder utilization than you would think.
- Many companies have started with this pitch and pivoted away:
- Collective Health started with this pivot, ended up going upmarket to larger tech companies (not "startups").
- Sana Benefits started with this pitch, and ended up pivoting to being a TPA and MGU with a highly opinionated plan design.
- Angle Health started with this pitch, and ended up pivoting to being an "instant-quote" Cigna wrapper.
- Yuzu Health started with this pitch, and ended up pivoting to operating health plans around direct primary care and point of service payment
- Many others have pivoted into the ICHRA space from this, including Pebble Health and Venteur."
[NK Note: Most startups don’t even know if their own business is working. Maybe just focus on that first.
They’re not going to innovate on their employee plan design when they have a million other things burning around them.]

The Smart Pill Bottle Conundrum
"I’m the former CEO/cofounder of TowerView Health, a VC-backed medication adherence company that was founded in 2014. TowerView focused on chronically ill patients taking 5+ medications by partnering with pharmacies to reconcile and sort medications by dose into medication trays which were mailed to the patients’ homes and then inserted into a smart pillbox that could remind patients if they didn’t take their meds as prescribed.
Despite seeing an increase in medication adherence from 70% to 99% in a clinical trial run by Penn Medicine and Blue Cross and contracting with 5+ health plans, TowerView shut down in 2019. Some thoughts on why so many founders start medication adherence companies and why none have really become sustainable businesses.
(Disclaimer: much of this is based on the market before 2019 and although nothing usually changes in healthcare that quickly, there may be some recent development since then that impact this analysis)
First, why do so many people start companies around medication adherence? (e.g., smart pill bottles/pillboxes, reminder/refill apps, etc.)
- It addresses a real problem that people can personally relate to. If you’ve ever taken care of your grandparents, have young children, or even take medication yourself - it’s easy to understand that taking medication is not easy. 125,000 people die per year due to medication non-adherence. This is a problem that needs to be solved.
- It’s a big market. Take market sizing stats with a grain of salt but the numbers are staggering: nearly a third of Americans suffer from at least one chronic illness (133 million Americans), 50% of patients don’t take their meds as prescribed, and non-adherence results in $300 billion of avoidable costs. If someone could increase adherence, it’s easy to see why payers, providers, pharma, caregivers, etc. would pay for it.
- Relative to many of the other problems in healthcare, the complexity of this problem/market isn’t readily apparent from the start. Speaking from personal experience, we were 23 when we started TowerView and naive to how deceptively difficult this problem is to solve.
So why is this a harder problem to solve than most people think? We’ll break it down into a few key questions:
Which problem are you solving? The root issues are complex: affordability, making sure patients take the right meds (reconciliation), prior authorizations, refilling/renewing the prescription, receiving the medications, side effects, forgetting to take the meds, understanding why the meds are necessary, etc. Most of the adherence products on the market today solve 1-2 of these problems, but that may not create enough value for a patient to use the product or someone to pay for it.
Who is your user–the patient or the provider? Designing for elderly and chronically ill patients requires a lot of consideration. These users are not traditionally tech-savvy, may not have in-home support, and are comfortable in their ways (i.e., resistant to change). If your solution involves the medication itself then you must account for pharmacy distribution which is highly regulated and optimized for the status quo.
Who pays and how does your solution get to your end user? This is usually the hardest problem to solve as each stakeholder is looking for different benefits and as of 2019 there wasn’t an insurance reimbursement for “adherence” tools. As such, you need to prove the value with each stakeholder/customer individually to get them to pay for the solution. Here is what we learned from talking to different stakeholders based on how they make money and what would motivate them to pay for a solution:
- Payers: Health plans mostly care about (1) quality scores like Medicare Star Ratings tied to refill rates and (2) reducing hospitalizations. The challenge with quality scores is that it is more efficient for payers to put members on 90-day auto-refills and reduce copays to $0 for the relevant medications. To pay for reduced hospitalizations, payers want proof in a pilot that increasing adherence results in a meaningful decline in medical costs (i.e., not just higher refill rates which is how payers measure adherence). Unfortunately, each payer will require a 6-12 month pilot with their own members to prove the value and even then it can take years for a full rollout. Finally, the biggest challenge with payers is that they don’t have a relationship with their members so it’s up to the vendor to get members to use the product which is essentially another sale to the end user.
- PBMs: Don’t even try. If payers need permission from their PBM to roll out your solution then run - PBMs will almost always try to block you or threaten to terminate their contact with the payer if they sense any danger of disintermediation.
- Providers: Health systems are primarily motivated to reduce 30-day readmissions. The challenge is trying to operationalize onboarding during patient discharge which is typically chaotic and not conducive to introducing new tools. If it’s not seamless and/or revenue generation (not just cost avoidance) providers are unlikely to go out of their way to use your tool.
- Pharma: The challenge with pharma is that their primary motivation is to increase refill rates for their own specialty medication. From a patient’s perspective, they could be on 5+ medications and view all of their medications as important yet pharma will only care about their medication. Similar to payers, pharma doesn’t have a direct line of access to patients so it’s challenging to get patients to use a product sponsored by pharma. The other challenge is that specialty medications usually cannot be repacked or altered from the original packaging, so there is little you can do from a hardware perspective.
- Pharmacies: The pharmacy serves as the best distribution point for patients as they have the relationship with the patient/caregiver. That being said, pharmacy margins are extremely thin with many chronic/generic medications for Medicare/Medicaid patients result in losses. Additionally, PBMs are siphoning off high margin specialty medications and imposing fees (e.g., DIR) that make it very challenging for retail pharmacies to operate profitably. Ultimately, if pharmacies are losing money on chronic prescriptions then they are not financially incentivized to increase adherence for those meds.
- Caregivers: Now that we’ve gone through all of the traditional healthcare stakeholders, we’re left with the consumer pitch–sell to adult children who are taking care of their again parents. This is a growing market, however, you’re selling a luxury product as most people will expect their insurance to cover anything “health” related. Admittedly, this is the market I know about the least, however, we haven’t seen any of the traditional consumer products in the space take off (yet!).
Finally, the last thing I’ll say is that there is a lot of fatigue in the market over medication adherence products. Even the fact that Nikhil asked me for my thoughts is an indication that investors and healthcare companies have heard a million different pitches for smart pill bottles/boxes, reminder apps, etc. and it’s hard for them to get excited when there is a “graveyard” of adherence companies. That being said, for every Webvan there is an Instacart and all of the TowerView alums are rooting for the startup that can figure it out!"

[NK note: Got enough questions about why this was a bad idea that I voluntold Rahul he had to write this to save some biomedical engineering students.
One thing I hear a lot about this idea is that Remote Therapeutic Monitoring (RTM) codes make this a more viable business today because providers can bill insurance for providing smart pill bottles and interpreting the data. Personally, I think the RTM/RPM codes for this will probably get clamped down on but I could be wrong.
I’ve never REALLY thought of medication adherence solutions as a full fledged business and more of a feature of existing businesses. Happy to hear why I’m wrong (as per usual) and think Rahul’s analysis still stands today].
Referral Management and New EHRs (again)
"There are no bad ideas, just bad timing! Here are a couple of ideas that many great founders have tried but just may not have had their moment yet…
Referral Management
100M+ specialist referrals occur every year (source); many are sent to the wrong type of specialist the first time, involve months-long lags for appointments, and/or result in patients showing up at the specialist office without the appropriate documentation and insurance requirements. Money and time are wasted, appropriate care is delayed, and physicians and patients have a terrible experience.
It's one of the most enticing problem spaces out there (the potential for a specialist marketplace! analytics on physician performance and availability! network effects!), but multiple generations of companies (including mine) have tried and failed to get to scale in addressing this business opportunity, and referral processes still suck.
Navigation companies have certainly proliferated, but they are really a superficial bandaid in the form of concierge services and read-only steerage apps, versus something that should be embedded into real-time, point-of-care workflows. With the rise in risk-bearing primary groups who are financially on the hook for wasted or higher-than-necessary specialist spend, and better infrastructure for interoperability, summarization, and routing, will the stars finally align for someone to build an important company in this space?
[NK note: 10 different companies with proprietary quality scoring models and yet all of them tell you that the best specialist is at *checks notes* the Mayo Clinic.]

Modern EHR (see "The Six Stages of Health Tech Grief", by Nikhil Krishnan)
There have been countless attempts to build modern EHRs targeting traditional outpatient clinics, virtual care providers, and value-based care groups, but we've yet to see any company get to venture scale in the last couple of decades. And how many VC dollars are spent by early stage care delivery companies rolling their own EHRs because they can’t find a great off-the-shelf option? (hint: way too many) Few founders (none?) are masochistic enough to attempt to build a platform that sells against Epic, but imagine if hospitals had at least one other solid option out there to choose from...
But now, the Meaningful Use halo effect has dissipated, the fundamental business and operating model of healthcare is changing in a way that will soon make legacy EHRs obsolete, and AI advancements now allow for the fundamental rethinking of how humans interact with and leverage technology. Might we finally see a hyper ambitious founder, with an AI-native technology strategy that addresses both the outpatient AND inpatient opportunity, and a clever but aggressive go-to-market motion (e.g. starting in a severely underserved segment of the market that *isn't* dominated by Epic today, and then moving upmarket from there) build THE dominant, next generation EHR? It would require a lot of patience, capital, patience, luck, patience, and grit… but If I don't see a new entrant give Epic a real run for its money in my lifetime, I will die a discontented woman."
[NK note: 2 different people said don’t do new EHRs. This is the modern equivalent of putting your enemies head on a stake to warn you.
Please read this (along with the other ideas I hear), I will save your life.]

—
NK Conclusion
A lot of previously tarpit ideas can become successful if there’s a good “why now” reason. Honestly for several of these, AI might legitimately be a reason things could work today.
But make sure to tease out which problems are fixables operational challenges or related to the economics of the business, and how many things are related to ideologically or cultural things that may not have changed. It’s way harder to change the latter.
Hope this gives you a heads up on where the tarpit is at least.
Thinkboi out,
Twitter: @nikillinit
Other posts: outofpocket.health/posts
--
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







