Healthcare should NOT be local
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
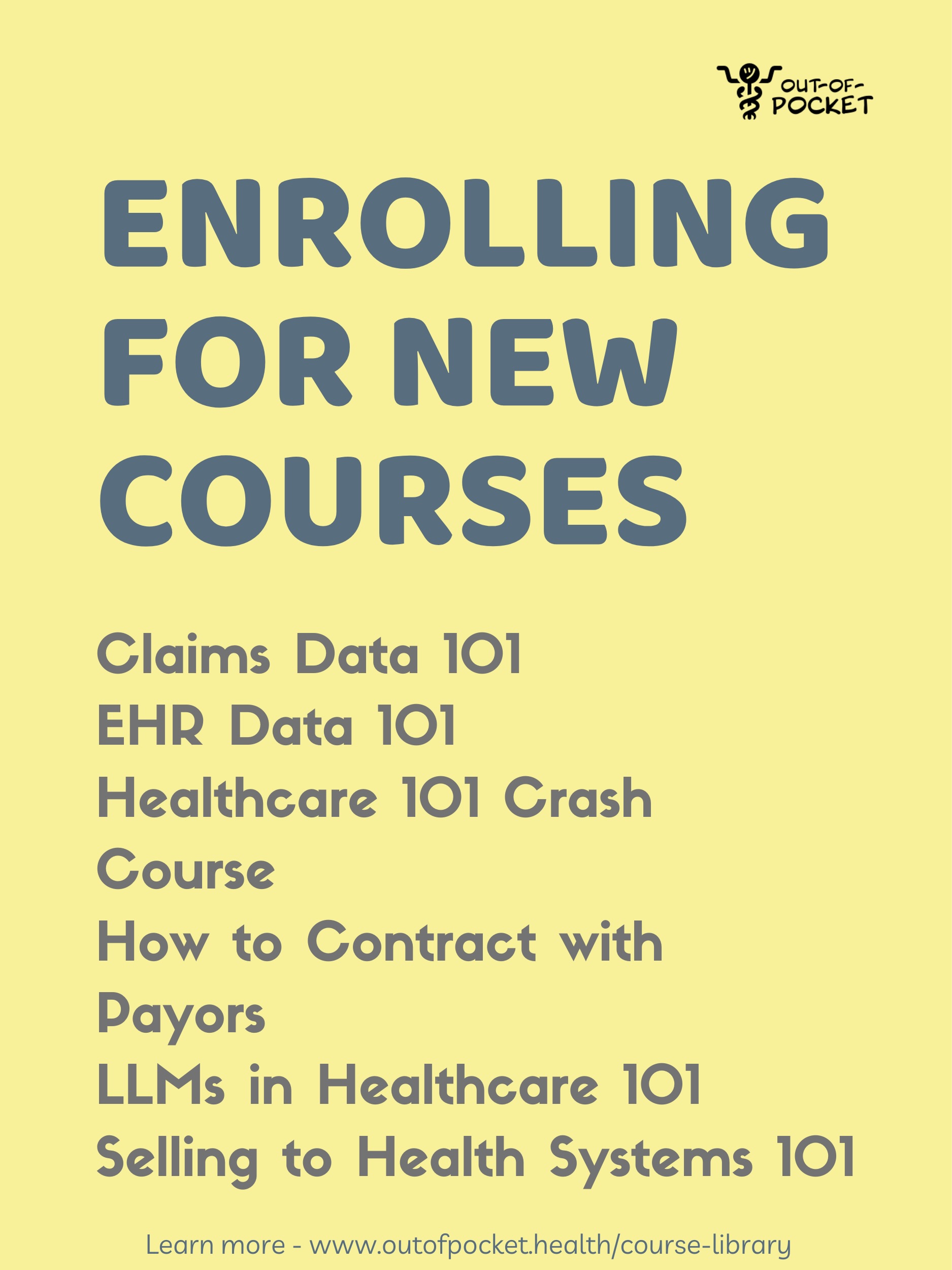
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
An idiom I’ve heard oft repeated is “healthcare is local”. Someone will say that on a panel, everyone in the audience nods, a single tear is shed from someone clapping really loudly.
But, I mean, maybe it shouldn’t be?
The pandemic has opened the door for us to rethink what parts of healthcare should be localized and what parts should be nationally or even internationally competitive.
Local grown…local owned
Right now when you sign up for insurance, your in-network providers are going to be local to the state you live (for the most part). There are a few problems with the fact that care is forced to be local.

One is the pricing power hospitals have due to consolidation, which I have talked about at length previously. Some ways hospitals can exert leverage due to care being localized:
1) A hospital has the top (or only) specialists in a lot of high need disease areas for that geography.
2) A hospital has access to some of the only available facilities and equipment that you need. If you want to go down the rabbit hole of another piece of outdated legislation, check out “Certificate of Need” laws. This is where new facilities have to prove to the state that there isn’t enough of X equipment in the state before you’re allowed to build a new one. Shockingly, states with those laws have less competition and have higher costs for procedures using equipment subject to those laws.
3) A hospital has way more control steering the patient towards their own services (e.g. by owning a lot of primary care providers who then refer patients to other in-house hospital services).
The goal of this local leverage is to get higher reimbursement rates from insurers, specifically commercial insurers and large local employers that are in self-funded plans. Because the dynamics of each market are so different, you’ll see extremely wide price variations between states for the same procedures

The other problem with keeping care local is you’re limited to the expertise of physicians within your state. But what if radiologists where you live tend to be way worse than in other states? What if no one at the local hospital has experience dealing with your disease? What if there are just not enough doctors or nurses in the area and the doctor:patient ratio is terrible?
These can be particularly acute in rural areas, which struggle to get physicians interested in moving to these areas. “Healthcare is local” is something people say when they have access to great care locally.
Finally, forcing people to keep care local can be tricky if you don’t want others to potentially know you have health issues. What if you’re in a small town but don’t want people to know you’re getting therapy? Or want to be a part of an addiction rehabilitation group that isn’t comprised of people you might see in your everyday life?
So even though there are nuances to delivering care based on local conditions, the idea that most of our networks are largely designed to get everything done locally is outdated.
Getting out of town
We’ve seen hints of local care being upended.
Self-funded employers have been exploring different ways to break up the issue of being confined locally. In extreme versions, this includes sending employees across the border (North or South) to get much cheaper prescription drugs. This is pretty silly considering it’s literally the same product here and there.

But in areas like healthcare services, surgeries, etc. it actually does matter where you get the care.
Walmart has been trying something interesting with its Centers of Excellence program, where Walmart will fly its employees to 9 of the best hospitals in the country if they’re getting a major surgery (spine surgery, different cancer surgeries, transplants, etc.) and fully cover the whole thing. While the surgery itself is more expensive, Walmart saves through avoided unnecessary surgeries, shorter hospitals stays due to faster recovery, faster returns to work, and a lower chance of readmission to the hospital.
Amazon has a similar program for their employees diagnosed with cancer to travel to City of Hope in Los Angeles.
The other area is telemedicine, which is slowly trying to take on the low-acuity issues or lifestyle changes associated with chronic care by connecting a patient to any doctor/coach across the country. But until now, actually getting people to use these programs + enroll has been tough and required a lot of local nudging (e.g. putting fliers in employers offices).
Smarter, national networks
Instead of thinking of provider networks as “which hospitals in my area are in-network”, we can build smarter network designs that figure out which parts of care should be local in-network, and which parts should be nationally in-network.
One of my favorite slides in the recent deck from Julie Yoo at Andreessen Horowitz is the idea of creating an insurance product that acts as a care coordination to the ideal level of care across the country. This makes me think of having virtual HMOs, where you see a virtual primary care physician that routes you wherever you need to go in-person as needed (virtually, in your area, or to a high quality health center somewhere else in the country).

COVID is enabling a lot of the changes that would enable the design of these smarter networks:
- Licensing for MDs will hopefully loosen up so they can practice in any state
- Telemedicine is becoming more normalized and we’ll have a better sense of its limits and where it’s as good as an in-person visit
- There’s now more flexibility of having a telemedicine visit without needing an in-person visit
- Remote work is leading to more geographic spread of employees leading to less leverage for an employer in a given geography
- Telemedicine has more clear reimbursement, including new CPT codes to reimburse for different remote monitoring activities
Smart networks for us to assess in a very detailed way the cost-effectiveness of care done locally vs. nationally vs. virtually. Should you be able to get a second opinion anywhere? Yes probably. How about primary care? That can also be done mostly remotely by a physician, but maybe some confirmatory questions are answered by someone that you see locally or a test administered via remote diagnostics. ER visit? Has to be local.
I’m still thinking through this but my hunch is that local care should be things like:
- Anything related to social determinants (food, housing, etc.)
- Any non-invasive testing
- Emergency services
- Anything requiring frequent drug administration, dialysis, etc.
Vs. geographic agnostic care should be:
- Low-risk diagnoses
- Second opinions
- Elective surgeries
- One time curative therapies
Obviously I haven’t bucketed every single item, but if you’re a health insurance carrier or an employer maybe you should. If you’re an insurance carrier and have a good sense of the cost/quality for providers across the country, why not create smarter provider networks?
New Practice Design
Insurance carriers would be the ones to design these smarter networks, and if I were someone like Oscar this is exactly what I would do. I think their new $0 virtual primary care offering is a really interesting wedge here. Most patients listen to what their doctor says for follow-up care, so if you can get a large number of patients actually using the primary care function, you can more reasonably launch a virtual HMO.
Oscar already has doubled down on narrow networks in each of their individual city markets; it could be interesting to rethink this as narrow NATIONAL networks instead. Considering they already have a joint insurance plan with Cleveland Clinic, is it that crazy to think about them using that to turn the Cleveland Clinic into a Center of Excellence that they fly patients from other cities into when needed? Or get virtual consults from specialists there?
On the one hand, an insurer can look across the country and try to design a good national network that can also load balance correctly (e.g. can’t send too many patients to the same place at once). On the other hand, Livongo could just build and manage that network themselves on behalf of an insurer. Looking at their latest M&A presentation suggests that’s the direction they’re moving, even talking about “virtual Centers of Excellence” for specialists.

Or maybe you’ll starting seeing virtual multi-specialty groups? Interesting thread here that examines what it might look like.
One of the big open questions around creating smart national provider networks is being able to identify high quality providers/physicians. For example: Walmart has partnered with Covera Health to identify high quality radiology groups and send employees there to avoid misdiagnoses.
Having better ways to identify high quality providers/physicians still seems like a gap that would need to be filled to actually do this. Instead of sending everyone to the same brand name hospitals, we could find smaller Centers of Excellence across the country that specialize in one really specific area (e.g. joint surgery) and do it much more cheaply than the brand names for better quality.
Idle Musings and Parting Thoughts
Some other random things that come to mind when I think about this:
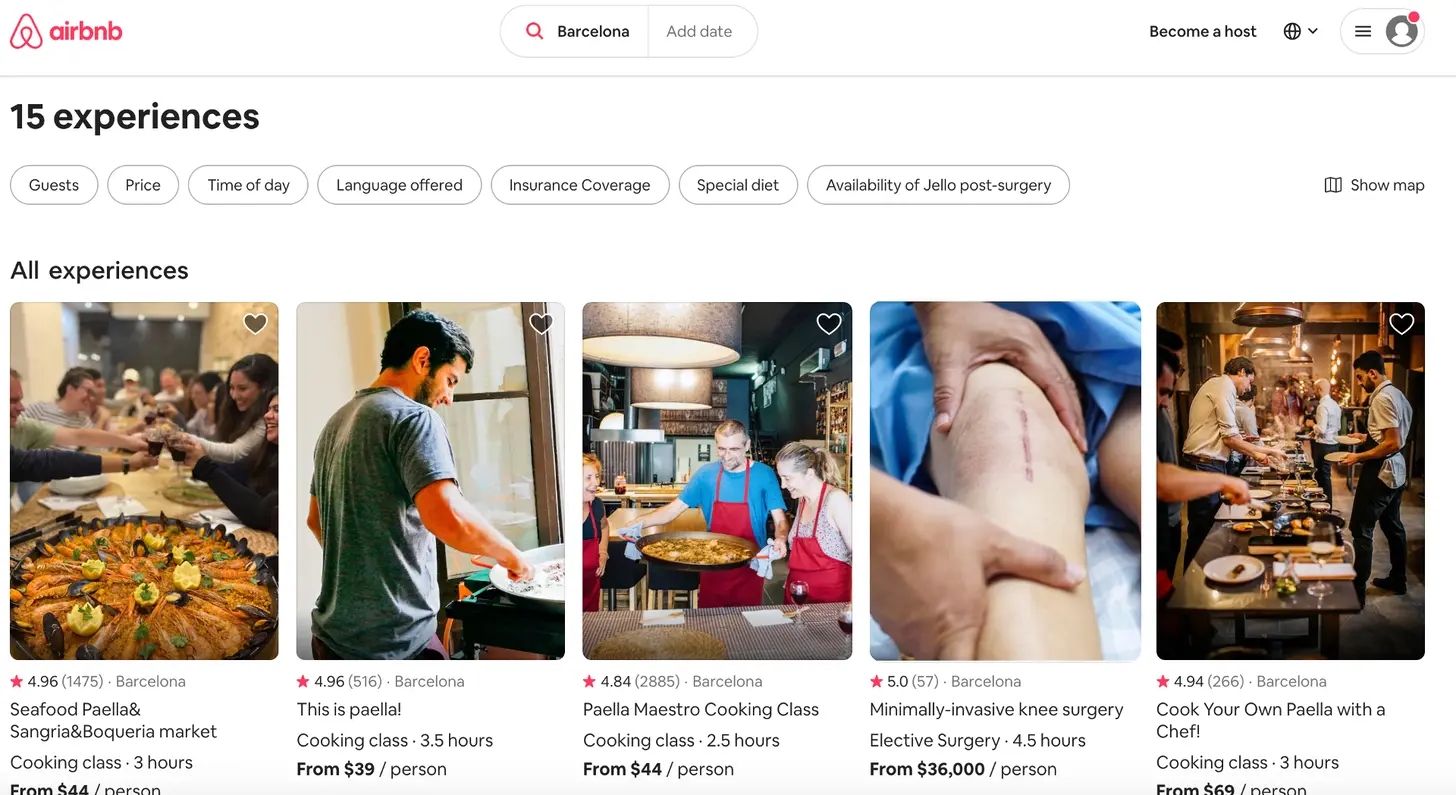
- I wonder if we’ll see more/new medical tourism bundles. Going abroad for surgeries isn’t a new concept, but there’s probably some room for new players with updated branding. Especially as Airbnb/hotels and airlines look to bounce back, maybe there’s an opportunity for them to work together with hospitals on medical tourism packages.
- One of the nice things about traveling today is there are a lot of standards - I can use the same ridesharing app wherever I go, the Westin is the same basically everywhere, I can use my ClassPass points there, etc. Healthcare does not have this, and instead anytime you move or switch health insurers you need to rebuild everything. One thing I like about One Medical is it provides a standard I can expect (in any city it’s in). With fully virtual specialty groups, we might be able to create consistency wherever you go regardless of their local presence.
- How far are we from surgeons opening fully telepresence ambulatory surgery centers for low-risk procedures? This paper assessed usefulness of a telepresence robot in the operating room of a a level 1 trauma center and it seems not bad? Then again I’ve seen how mad I get when there’s lag and I lose a game of Super Smash Bros. online, now imagine the stakes are higher…

Honestly I have no idea if patients would even want a national network, but it would be interesting to see someone lean into the opportunity that COVID has opened and try it out. It’s worth noting that Walmart’s Centers of Excellence was optional until it required employees to use it in 2018. The same might have to be required of patients that opt into this plan for it to work, but if the pricing for patients were attractive it might work.
Thinkboi out,
Nikhil aka. “Center of Inferiority”
Twitter: @nikillinit
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.