Is healthcare private equity that bad?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveNetwork Effects: Interoperability 101
.gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
New Discussion Post
Today I have a new post and discussion topic.
To reiterate the rules:
I’ll pose a question and give my thoughts. In a future newsletter I’ll include ~3 of my favorite answers people reply with. I’ll possibly even make a meme related to your answer.
Good answers are ones with a novel viewpoint, data to back up their claim, personal stories, and avoid clearly shilling something.
Please reply to this email with your thoughts on the question and let me know if you want to have your name included or be anonymous. You have to be on the newsletter to submit a reply to it obviously.
Try to keep answers to two paragraphs or less please. This obviously doesn’t apply to me because it’s my newsletter and these are house rules.
Is private equity in healthcare bad?
There’s been a ton of articles written about how bad private equity (PE) is in healthcare. It's hard not to hear some of the stories about serious understaffing at PE-owned facilities and the patients that get hurt in those scenarios.

But I’m left with an open question that I would love your thoughts on. Is private equity uniquely bad? Below are some very half-baked thoughts I’m trying to organize. Or am I half-baked and the thoughts are fully formed?
Share with me your thoughts on private equity in healthcare (good or bad), stories you have from private equity owned businesses or ways you think we can improve the use of private equity in healthcare.
Private equity vs. hospitals
I already know with this title I’m gonna get flamed a little bit. And to be very clear I’m not going to die on the hill defending private equity. I have much worse opinions, believe it or not. Like I think Succession is a bad show.
I think there’s lots of things PE does that’s bad. But I think the things that private equity gets criticized for are basically the same things that hospitals do.
Price/utilization - A private equity acquisition increases service prices and pushes for more procedures. They’re going to get their pound of flesh…acquiring procedure-heavy derm practices. Mohs money, Mohs problems.
But…hospitals are notorious for buying physician groups/other hospitals, adding fees, and jacking up prices on commercial health insurance using the extra market power.
I found it difficult to determine if utilization increases after a hospital acquires another hospital. It seems to increase with things like skilled nursing facilities when they own them. Also an older study suggested higher intensity cardiology services increased post-acquisition. I think the fact that physicians who work at health systems have their compensation tied to a system that incentivizes procedures suggests there’s already some pressure to do so.
Referrals - PE-owned practices tend to refer to ancillary service providers (e.g. pathology labs, billing services) that the PE shop owns, which are much more expensive.
But…hospitals quite literally acquire or affiliate with primary care physicians because they generate more than $2.1M in revenue for the hospital thanks to downstream referrals, testing, etc. to the main hospital system (source: Merritt Hawkins). In fact, hospitals will sometimes put contracting language + much simpler tools for internal referrals.
“Federal rules generally block hospitals from directly tying physicians’ pay to referrals, because of worries that factors other than patient needs could impact physicians’ decisions. Doctors and hospital officials said that hospitals make the goals clear in ways both subtle and overt.
Some hospitals have employment contracts that mandate doctors refer within their system, with a few exceptions required by law. In electronic medical records, a system’s own specialists and services are sometimes located in a convenient drop-down menu, while referring to an outsider requires additional steps. Hospitals may train doctors’ staff on where to direct referrals, since doctors often leave the final decision to them.” - Wall Street Journal
Ah, yes, a functioning system where the convenience of drop-down menus is responsible for some of the most important care decisions in a patient’s journey.
Funnily enough, I asked a few PE friends about this and they all separately said that most practices they look at end up violating anti-kickback/referral laws by accident when they do referrals. This is largely because of how complicated the laws can be. And actually the PE shops try to avoid those deals because as they roll them into larger entities, they come under more scrutiny. I mean this is coming from the PE people themselves, so take it with a grain of salt.
Yes I have some PE friends. Who’s going to take me out to drinks in a down market? Call that hedge fun.
Staffing - Private equity increases the ratio of patients to clinicians to near unsustainable levels.
But…all of the nurse strikes happening across the country are due to staff ratio issues at hospitals and bills are being proposed to force hospitals to adhere to a staffing standard.
Outcomes - The research on whether private equity makes outcomes worse is pretty mixed and hard to assess. It seems to skew towards improving or maintaining quality measures when you look across the board at practice or hospital acquisition, but potentially worsen for areas like nursing homes.
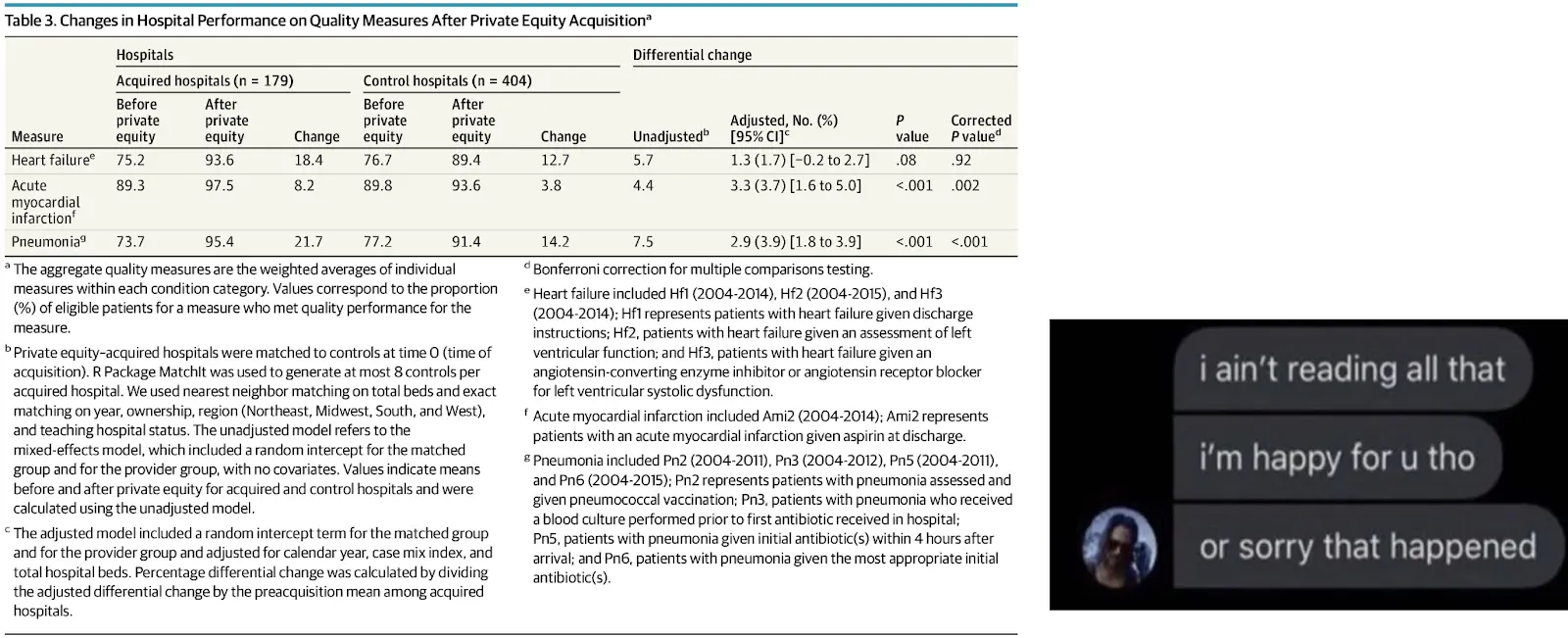
But…simultaneously a lot of the new papers about hospital mergers show a decreasing quality of care. This is important because one of the main pushes for hospital consolidation when the ACA was passed was that it would improve quality of care under one roof. Narrator: That was a lie.
The answer to PE and hospitals here is probably “it depends” on whether they make outcomes worse once they get involved. And that depends on whether or not I have the patience to read the full studies.
—
A few things do seem somewhat unique to private equity. I think a key distorting mechanism is an aim to return money in a 3-5 year time frame. This not only means the changes happen relatively quickly but also pushes the aggressive use of debt. That can accelerate the demise of targets bought if management doesn’t execute, if the macroeconomy changes, if AI escapes the box and kills us all, etc.
But it’s not like private equity WANTS things they buy out to fail. There’s obviously a bigger upside when they succeed, but they have the appetite for more risk relative to hospitals so they’re also going to have more failures as a result. Unfortunately, patients and physicians get caught in the crossfire there.

I also think private equity targets areas where they can have more control over taking patients with “richer” insurance plans and avoid patients that are low-income or have bad insurance. Whereas hospitals generally have no choice but to take lower-income patients, but then use other mechanisms to make money from that fact (e.g. 340B pharmacy programs). Plus hospitals make real estate expansion decisions and partnerships with companies like One Medical to get referrals from those patients with good insurance plans anyway.
Private equity seeks out system-level incentives
I don’t think the fact that other entities do these things makes it “okay” for private equity - but the evidence suggests that it’s a system that incentivizes all these behaviors. Or it’s a system-wide problem that everyone is facing and adapting to (e.g. staffing). Private equity is simply one actor in it. So it’s once again a question of what outcomes do you want as a healthcare system and what incentives should we add to the system to get there.
If you ever want to figure out where there’s money to be made in healthcare and how it’s made, just look at where private equity flocks. They’re so ruthless and fast that it’ll happen way quicker and earlier than hospitals/payers. This principle can also help guide regulatory fixes. This genuinely excellent whitepaper calls private equity a “divining rod” for financial incentives in healthcare.
For example - many private equity companies bought physician staffing companies like Envision and TeamHealth which used to bill out-of-network charges for things patients couldn’t choose like anesthesia during surgery. This is clearly a bad thing societally! So it took a while, but we passed the No Surprises Act and essentially rekt those business models.
It’s not always “negative”, per se. Participating in value-based care generally requires quite a bit of investment upfront, and private equity is a tool that’s been very useful in this area if it’s lucrative enough. There’s a lot of investment in Medicare Advantage - here’s an example talking about CareMore and how private equity allowed them to scale and hit quality metrics (that coincidentally would also get them paid more).
“CareMore was acquired from its physician-founders by the private equity firm CCMP Capital in 2006, and then sold to a large public health care company in 2011. During the period of private equity ownership, CareMore increased from 4 to 27 care centers and from 22 000 to 55 000 patients, all cared for under capitated payment models. Data from the Centers for Medicare & Medicaid Services (CMS) suggest that care quality improved under private equity ownership.
Rates of colorectal screening increased from 56% in 2008 to 74% in 2011, the latter compared with a national average of 58% that year. Hemoglobin A1c and blood pressure control followed similar trajectories, with rates 10% and 20% above the national average, respectively, in 2011. When CareMore was sold by its private equity investors in 2011, it was in the top third of health plans according to CMS quality rankings for Medicare Advantage plans.” - JAMA
If you’re in the camp that Medicare Advantage is a positive step in value-based care, then this is good right? PE is a tool that follows the metrics and money, the key is setting a system that rewards that.
Private equity = “big companies”. We need more community businesses.
I think most of the issues people have with private equity in healthcare are really issues people have with companies becoming large. When companies become large, they end up defaulting to metrics and measurable things to evaluate people, divisions, etc. It’s somewhat impossible to run a large company otherwise; the organization is too complex and requires people to move in a unified direction guided by metrics. It doesn’t help that most large companies are financed by investors with a fiduciary duty to return money in a specific time frame which adds pressure on which metrics to choose.
The intangibles are what you lose as you move to one of these more metrics-driven organizations. This is happening across all industries, it’s not just healthcare. But I think this is uniquely pronounced in healthcare because:
- A lot of the things doctors do is out of altruism and thus make them easy to exploit. Physicians who feel pressured to do more surgeries try not to leave their other patients hanging even if it requires uncompensated time.
- Healthcare has third-party payers (health insurance, etc.), opaque pricing, and patients don’t know how to evaluate the service providers they’re going to. This is ripe for shitty providers to fly under the radar, for patients to get bamboozled into getting things they don’t need, and to milk the system for all its worth.
- A lot of the things that patients want and feels like good care is usually inefficient. It’s spending longer with patients than they need, it’s proactively checking in on them even if it’s not billable, it’s having arts and crafts sessions and community events at the nursing home. A system that squeezes efficiency will lose these things. I mean the idea of Relative Value Units quite literally tries to measure physician productivity, gives more weight to procedures and less to patient face time, and ties all that to reimbursement. This isn’t theoretical.

At the end of it, this is why I think it might be better to have way more small practices and businesses instead of large companies in healthcare. Small business owners care about intangible things that will never show up in those metrics: their reputation and standing in the community, the quality of the service they deliver, what their peers think about and say about them. A lot of those things are counterbalancing forces from bad behavior.
As companies grow larger, decision-makers get further and further divorced from the end patients and operate with different incentives. Then the consultants and optimizooooorsss come in and shit really hits the fan. Keeping decisions made with people that sit closer to the patients would be better for everyone IMO and would address some of the shortcomings people have with hospitals AND private equity. That’s why I’ve also advocated pretty heavily for physician independence.
For what it’s worth, I don’t think it HAS to be this way for large companies. One Medical is a large company and has had a large PE investor (Carlyle Group), but as a customer it never felt soulless to me. Oak Street still seems to have a solid NPS despite growing a ton. I’ve heard anecdotally from friends that the PE-owned fertility clinics felt like a much better experience vs. the independent or hospital-affiliated ones. But I think keeping the intangibles requires very deliberate management choices to maintain that, or they’ll naturally disappear as metrics take over. KPI actually stands for Kill Personable Interactions, most people don’t know that.
Some potential fixes
I think we should encourage investing in healthcare, which includes private equity. But I think there are some things we can explore to improve things and make sure it’s not harming patients.
We need more data: In a previous life I’ve had to try and map private equity ownership to providers and it sent me into the next life. Just look at the methodology for this paper to answer the question “what happens when private equity owns a practice?”. It’s longer than the damn paper itself!
- Use one dataset to identify PE ownership
- Find 2 separate datasets to identify physician/practice affiliations
- Probabilistically link those datasets together
- Get access to claims data
- Try to link that but it’s de-identified
- Outcomes data is impossible to connect and ancillary/advanced practitioners (e.g. optometrists and nurses) bill differently so aren't included. Despite staffing changes being a key strategy for PE acquisitions.
This has severe limitations and makes it extremely difficult to scrutinize the industry. We need data on ownership and we need data that can monitor practice and referral patterns much more easily.
New financing options for companies: I’ve talked about this a lot in the “Digital health needs more creative financing options” post. But I think in particular for physicians that want to sell their practice, PE or hospitals feel like the only options. I talk about succession loans as another alternative to explore, as well as other financing mechanisms for growing companies that might be more palatable to physicians or operators of any PE-targeted healthcare business that doesn’t want to sell to them.
Revising corporate practice of medicine laws, AKS/Stark laws, and physician-owned hospital laws: These are a plethora of laws that prevent financial interests from interfering in physicians practicing medicine. While well-intentioned, what this generally means in practice is “which large companies have the best lawyers to exploit the gray space in these laws”. This essentially shifts the financial upside and control to owners like private equity instead of physicians themselves.
I think physicians are incentivized in the same ways as the hospitals and PE shops so it’s unclear to me why they should be excluded from ownership. Their desire for status/seeming ethical to other physicians and risk of losing their license would probably be better at mitigating bad behavior. Something I’ve argued about in the past.
More penalties for rule breaking - I think most private-equity shops navigating the gray area are calculating (expected probably of an audit) * (the size of the penalty) vs. the amount of money they’d make doing X behavior. I think either you need to increase the scrutiny into these companies which might come from better data, or you seriously increase the size of the penalties to then force the companies to better self-regulate.
Conclusion + parting thoughts
Please don’t label me the “pro private equity guy” because I don’t want my head to end up on a stake. I’m just honestly trying to sus out in a somewhat objective way where PE is bad and where it can have more guard rails. Some final thoughts:
- I think a big reason PE gets scrutinized more than hospitals is that hospitals portray themselves as NEEDING to do these maneuvers to survive off low margins whether or not that’s actually true. Private equity on the other hand seems like a bunch of rich people trying to get richer. It doesn’t help that all the private equity firms are named “3 Dude’s Last Name Partners” and the hospitals are “Holy Sisters Helping The Poor And Needy.”
- Remember that this comes from the PE people, but most of them agree that you don’t want to make doctors do things they don’t want to do after you acquire them. It tanks the practice if the doc leaves or the patients don’t come back. The private equity shops view themselves as trying to take stuff off the doctor’s plate they don’t want to do (back-office + things they can shift to other clinical staff).
- On that note, isn’t it kind of amazing that the owners of practices, nursing homes, etc. who choose to sell don’t really get that much shit in the press coverage? Some amazing PR jiu-jitsu there.
- I think venture-backed businesses have largely managed to look less like ruthless PE businesses because they didn’t have to return money in <5 years, were on a much smaller scale, and the VC firms weren’t literally running the business. As these companies need to reach profitability, I think we’ll see more stories and behaviors from these VC-backed companies that look like regular PE-owned providers. The fair trade coffee beans are out, the Keurig is back in.
Anyway, tell me your stories and thoughts about the role of private equity in healthcare. I’m happy to change my mind on any of the points above. I’m especially interested in hearing from PE people or healthcare businesses bought out by PE as well (I’ll keep you anonymous if you want).
Thinkboi out,
Nikhil aka. “PE people please don’t claim me I still don't like most of you from a personality perspective”
Twitter: @nikillinit
Other posts: outofpocket.health/posts
Thanks to Bradshaw Kenimer for reading drafts of this
---
Featured Jobs
Sign up for the featured tier in the Talent Collective to get your jobs in the newsletter, on Twitter, etc.
- Arlo is building a value-based health plan for small and medium-sized businesses. They're hiring a head of care navigation.
- Red Scissor makes it easier for patients to get their complex prescription drugs. They're hiring a pharmacist lead.
- Curana Health is a value-based care platform for long term care and senior living. They work with 1,000 senior living community partners across 25 states, servicing over 100,000 patients annually. They're hiring a VP of Data Strategy.
---
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!!
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
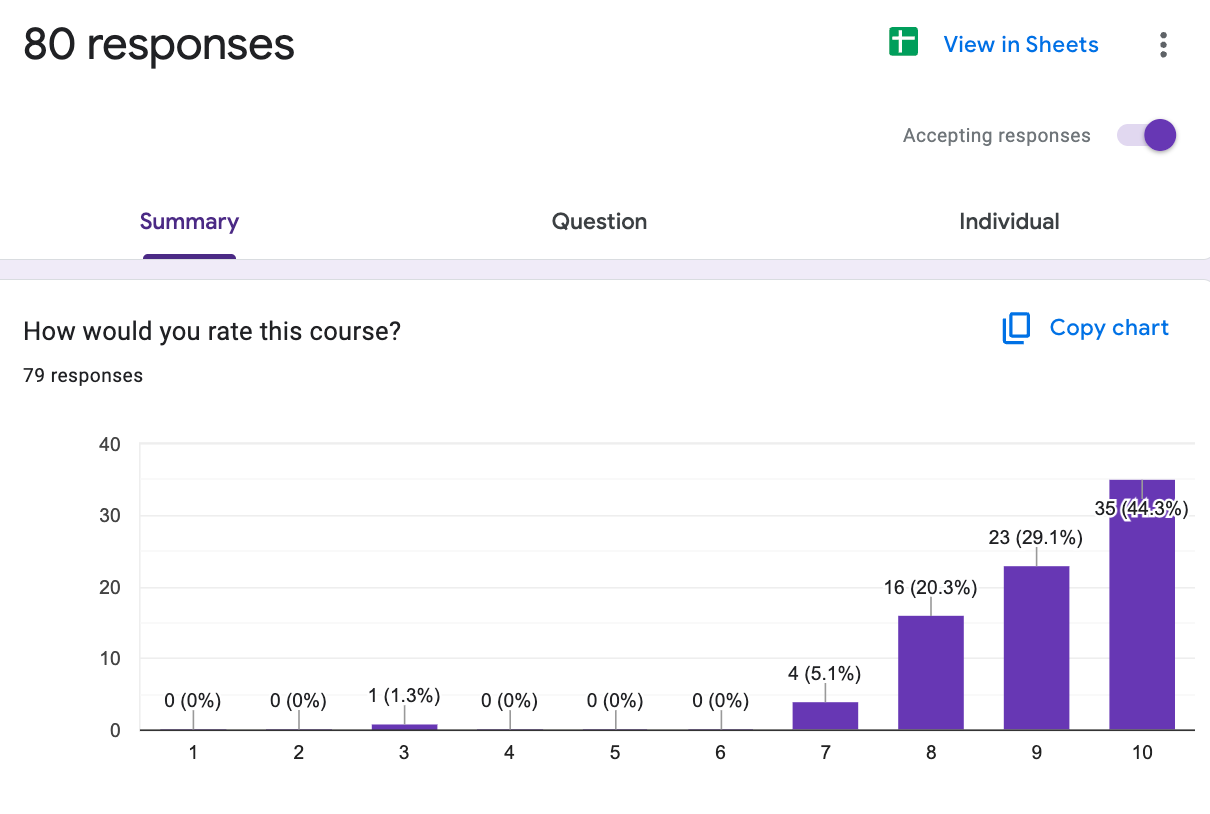
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
Selling to Health Systems (starts 10/6) - Hopefully this post explained the perils of selling point solutions to hospitals. We’ll teach you how to sell to hospitals the right way.
EHR Data 101 (starts 10/14) - Hands on, practical introduction to working with data from electronic health record (EHR) systems, analyzing it, speaking caringly to it, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →Our Healthcare 101 Learning Summit is in NY 1/29 - 1/30. If you or your team needs to get up to speed on healthcare quickly, you should come to this. We'll teach you everything you need to know about the different players in healthcare, how they make money, rules they need to abide by, etc.
Sign up closes on 1/21!!!
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.

Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







