Malpractice, Expert Witnesses, and Lawsuits with Dr. Eric Funk
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Today I’m interviewing Dr. Eric Funk, an emergency medicine physician and an expert in…experts! Specifically around expert physician witnesses used in medical malpractice suits, which he writes about on his newsletter, Expert Witness.

We discuss:
- How medical malpractice actually works
- Why cases go to trial vs. get settled
- How physicians think about testing and how it’s impacted by malpractice lawsuits
- Comparing medical malpractice in different countries
- Common mistakes made in malpractice cases
1) What's your background, current role, and the latest cool healthcare project you worked on?
I'm an Emergency Medicine physician, practicing full time at a Level 1 trauma center in the Midwest. I went to medical school at the University of Kansas and did my residency training at the Mayo Clinic in Rochester, MN. My most interesting project right now is my work on medical malpractice and expert witnesses. Medical records become publicly available once a malpractice lawsuit is filed, and I sort through thousands of cases to find good examples to educate physicians. I run the only business that publishes the actual, real-life records of what happened in the medical care, from the doctor's notes, to lab work and imaging studies. Then I show the behind-the-scenes of the legal process from initial filing of the case to the final dismissal, settlement, or jury verdict.
I also have a niche interest in the expert witnesses who write opinions for these trials. Physicians command very high consulting fees for these lawsuits, which has incentivized some bad behavior. There are many examples in which a plaintiff's attorney simply has to pay a high enough fee to a physician, and they will sign off on any corrupt and uninformed opinion. Mine is the first publication to actually show the real-life expert witness opinions for scrutiny by the general community of physicians.
2) What are the most common reasons patients tend to sue physicians, and what ends up getting looked at to see who was in the right or wrong?
Most lawsuits revolve around serious diseases that have very unusual presentations. For example, most patients who have a heart attack will present with chest pain, shortness of breath, or sweating. However, there is a small percentage of patients who have a heart attack but present with vague and unclear symptoms. A patient who checks in to the Emergency Department with nausea may not get testing for a heart attack and could easily be sent home, suffer a cardiac arrest and die. These situations are extremely rare but are not infrequent when multiplied across millions of ED visits every year.
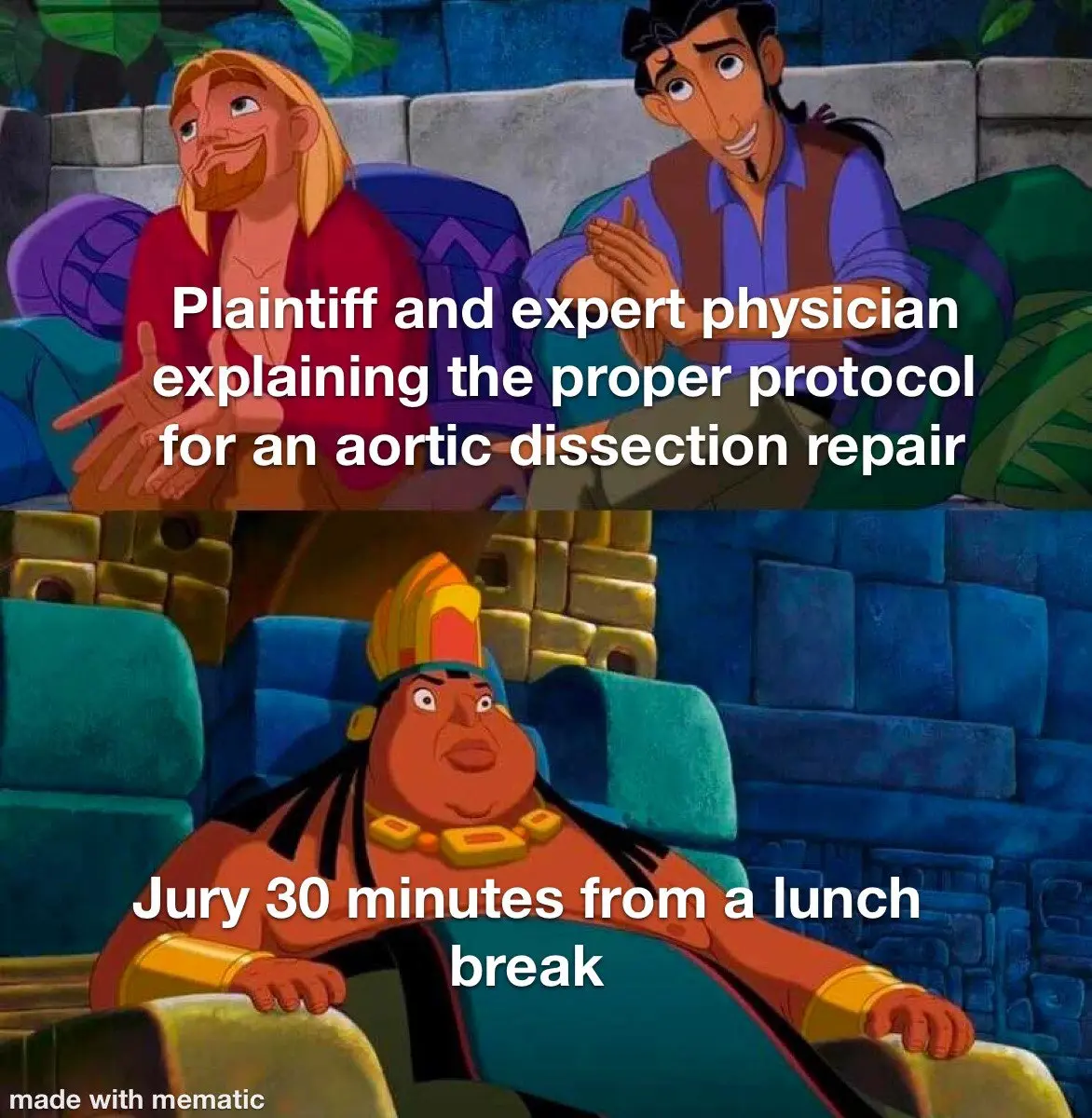
Theoretically, the doctor is judged by the "standard of care". The legal definition of the standard of care is nuanced and widely debated, but basically boils down to what a reasonable doctor would have done in a given situation. If no responsible doctor could have made the diagnosis or prevented the bad medical outcome, then the doctor should not have a legal judgment decided against them. However, the reality of medical malpractice trials is much more complicated. If the lawsuit goes all the way to trial, the physician is going to be judged by 12 people with no medical training. These cases are often medically complicated and require high levels of expertise to understand, but in the end, 12 average citizens will decide if the doctor was "right" or "wrong".
3) On your blog it says that it's rare that most cases actually go to trial. Why is that the case and which ones tend to actually go to court?
The vast majority of medical malpractice lawsuits are settled instead of going to trial. There are multiple factors in play here, including the physician's desire to show they did the right thing, the medical malpractice insurer wanting to minimize losses, and plaintiff law firms wanting to recoup their costs. Proceeding to trial is extremely risky for both sides. If the defense wins, the plaintiff's lawyers can easily have spent 6 figure sums and several years of time they will never get back. If the plaintiff wins, the insurer and hospital may be on the hook for millions of dollars. Both parties are incentivized to reach settlements within the insurance limits.
The vast majority of cases that do go to trial are won by the physician. This usually happens when a plaintiff has a very weak case but is unwilling to negotiate with the defense. If a plaintiff makes exorbitant demands and is unwilling to come to an agreement, the defense has a significant incentive to take the case to trial, where they will likely be successful.

The medical malpractice industry is opaque and hidden from the public eye, but plays an important role in the cost of healthcare in the US.
4) How does medical malpractice insurance actually work? Do you pay monthly premiums and have a cap per case? Is it for the year? How much does it usually cost/factors that go into the pricing?
Medical malpractice insurance costs vary widely by physician specialty. Some specialties are more prone to expensive litigation. For example, OB/GYNs are notorious for being sued frequently. Not because they are bad doctors, but because delivering a baby is an inherently dangerous process and the bad outcomes are... very bad. Babies who suffer severe disabilities during the birth process will require a lifetime of specialized care, which results in large settlements and verdicts.

Most physicians work in large medical groups, which will have a blanket policy covering all of the physicians in the practice. The practice generally pays for coverage based on some metric (number of physicians, number of patients seen, number of operations performed, etc...) and all the physicians are covered under the policy. Most physicians in these groups prefer to focus on the practice of medicine rather than the business operations, so are generally unaware of how much their malpractice insurance costs.
Physicians who practice independently will generally buy an individual policy. Several states mandate physicians to purchase insurance. Even in the remaining states, very few physicians would consider practicing without insurance.
Most insurance policies cover a certain amount per incident, and a maximum amount during a calendar year. As a rule of thumb, most will cover $500,000-$1,000,000 per incident and $2,000,000 - $3,000,000 per year.
5) Looking through some of these cases - there seems to be a dance of "do more testing to reduce potentially missing something" and "the more testing/imaging you do, the more likely you are to see something ambiguous that the patient could say you missed later". If you're a physician how should you think about navigating that balance?
There is a delicate balance between too little testing and too much testing. The risks of too little testing are obvious. If we don't order a test and miss a disease that was treatable (an early cancer, heart attack, appendicitis, etc...), patients can suffer bad outcomes and it's easy to criticize the doctor. However, the general public has a hard time understanding how too much testing can be a bad thing. We expose patients to significant amounts of radiation, discomfort, anxiety, and cost when we run tests. We find a lot of abnormalities that are of unclear significance. For example, a CT scan of the chest may reveal a small nodule on the patient's lungs. Is it something serious like cancer, or something benign like a lymph node or scar tissue? There's no way to get an easy answer, so the patient undergoes a biopsy. After the biopsy they develop an infection that spreads throughout their chest, causes sepsis, and they spend 10 days in the ICU before passing away. These situations are not infrequent.
[NK note: A paper looked at how many cascades of unnecessary tests caused harm to patients]

In general, most physicians err on the side of ordering too much testing. Being sued for not ordering enough tests is much more common than being sued for ordering a test and getting an ambiguous result that later turns into a serious diagnosis. The rates of testing, especially medical imaging, having sky-rocketed in the past decade. This is partially due to easier access to these tests, but also because no doctor wants to miss something on their patient. The fear of litigation certainly plays into this. A senior partner once told me "no one ever sends you a thank you note for not ordering a CT scan".
6) How do lawyers find expert witnesses? What criteria are they considering when they choose one? I'm guessing they have criteria they use to pick physicians that might "side" with them?
I'm not an expert on how lawyers find expert witnesses, but it seems to mostly happen by word of mouth. Some firms that specialize in medical malpractice have a short list of experts they have worked with over multiple cases, and they like to stick with them. There are several websites and services that let physicians advertise their interest in doing expert witness work. There are varying levels of success with these sites.
At the most basic level they are looking for a physician who has similar expertise and training as the defending physician. A long track record of leadership in the field, numerous publications, and teaching experience are also highly valued. Most experts do not end up speaking in front of a jury, but obviously an expert who is a polished speaker and communicates clearly (both written and verbally) is important.
The law firm generally will ask a physician to do an initial brief review of the case. The physician will communicate their basic opinion about the case (whether or not they feel the defending physician was negligent). If their opinion matches the law firm's purposes, they will then be hired for a more formal review and submission of a written expert witness opinion. In reality, there are numerous physicians who will write whatever opinion the attorney wants, as long as the price is right.

7) If a physician is thinking about becoming an expert witness, what are some things you've seen that trip up a new expert witness? How can a doctor be a "good" expert witness?
The most common error I see is writing an opinion about a doctor with different specialty training. If a neurologist is being sued, but a general surgeon is hired as an expert witness, the surgeon's opinion will not hold much weight. In some states, using an expert witness from a different specialty is enough to have the lawsuit completely dismissed.
Timely submission of the expert witness opinion is also critical. If the statute of limitations passes while the law firm is waiting for the expert's opinion, the lawsuit will be rapidly dismissed.
The law firm should be guiding the expert witness on these basic requirements, but it doesn't always happen. It's shocking to see lawsuits with potential for multi-million dollar settlements get thrown out for these simple errors.

8) How do other countries handle lawsuits vs. the US? Is there a particular reason why the US is so much more prone to lawsuits than other countries? Do you think it genuinely has a big impact on how medicine is practiced here?
The healthcare system in the US is uniquely dysfunctional compared to other countries. This is reflected in our medical malpractice industry. In Canada, physicians are insured through a program called Canadian Medical Protective Association. Most physicians are reimbursed by their Province for a portion of the costs. The CMPA is very aggressive in its defense of physicians. There are far fewer lawsuits compared to the US.
The frequent and massive lawsuits in the US are one of the numerous reasons healthcare costs so much here.
Risk of litigation (perceived or real) has a big impact on the practice of medicine in the US. It has slowly infiltrated every step of medical training, beginning from medical school. It is difficult to parse the exact impact, but the fear of lawsuits is now tightly interwoven into both the education and practice of physicians. Patients need to have recourse when they are harmed by the rare negligent action, but the medicolegal industry largely functions as a profits-first business that operates under a thin veneer of protecting patients.
Bonus: What's the funniest or most interesting medical malpractice lawsuit you've seen?
3 cases that will get a groan out of your audience:
1) A patient went in for a colonoscopy. The procedure did not reveal any polyps, there were no immediate complications, the patient went home and had no issues following the procedure. So why did they sue? The hospital realized later that same day that there had been a mix up between the "clean" and "dirty" scopes. The patient had undergone a colonoscopy with used equipment. The lawsuit was dismissed as there was no damage.

2) A female went to her aesthetician for a Brazilian wax. When the aesthetician removed the wax, she suffered a massive labial tear. She was rushed to the hospital with a large amount of blood loss and required a surgical repair. The aesthetician settled for a confidential amount.
3) A patient went in for a surgery to treat thoracic outlet syndrome, which happens when blood vessels and nerves are compressed where they exit the top of the chest. The surgeon thought he was removing the patient's first rib (an accepted treatment for this condition). Unfortunately he realized after the surgery that he had removed the clavicle (collarbone) and not the first rib.
Thanks again to Dr. Eric Funk, author of Expert Witness.
Thinkboi out,
Nikhil aka. “I plead the fifth”
Twitter: @nikillinit
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







