Pitching to payers, pilots, and what makes Blue Cross distinct with Tricia Garland
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
I get a lot of questions from people asking what health insurers would think about X, or if they'd cover Y. But I have hobbies, dreams, and other big questions I want to answer in my life that are not these.
So I decided to do this interview with my number one "hey-quick-question-what-do-you-think-about-this email forwarder" on the payer side, Tricia Garland. She runs the Strategy and New Ventures teams at Blue Cross NC.
We talk about:
- Not-for-profit vs. for-profit insurers
- What makes a good pitch to insurers
- Some deals she's worked on
- Challenges shifting to value-based-care
- and more

1. Background, current role and latest cool project:
I am responsible for the enterprise strategy and innovation teams and I am also a founder of the Blue Cross NC Diversified Business Group - aka “DBG”, which means I wear many hats. But my primary responsibility is building out DBG’s strategy, including determining what investments we should make next and ultimately making them happen, which means my teams:
- Identify and understand the key business challenges facing the enterprise
- Find business solutions for those challenges that address our goals of making health care affordable and accessible
- Execute ideas into sustainable partnerships or DBG portfolio assets
Since establishing DBG in December 2020, we have been busy executing transactions to protect affordability in our state. This includes our recent purchase of a market-leading TPA; that deal is the largest acquisition in Blue Cross NC’s 88-year history, expanding our capabilities and geographic reach.
Prior to Blue Cross NC, I was an advisor to pharmaceutical and biotech companies for acquisitions/divestitures and reimbursement optimization, giving me deep exposure to health systems globally.
In terms of cool projects, pharmacy is one of the next areas that my team and I are focused on. So, if you have ideas to disrupt the value chain there, I would love to talk! 😊
2. What makes a nonprofit different from a regular health plan and operationally how you think about your product strategy/roadmap? Are you a nonprofit the way hospitals are?
Blue Cross NC is a nonprofit that is here to serve our community, and is closely governed by our regulators to ensure that we do so. Our structure and community-driven governance makes us distinct from both for-profits and nonprofit hospitals.
For-profit payers: You will hear similar language from for-profits that you hear from us: focused on affordability, health of our members, purpose, equity, etc.
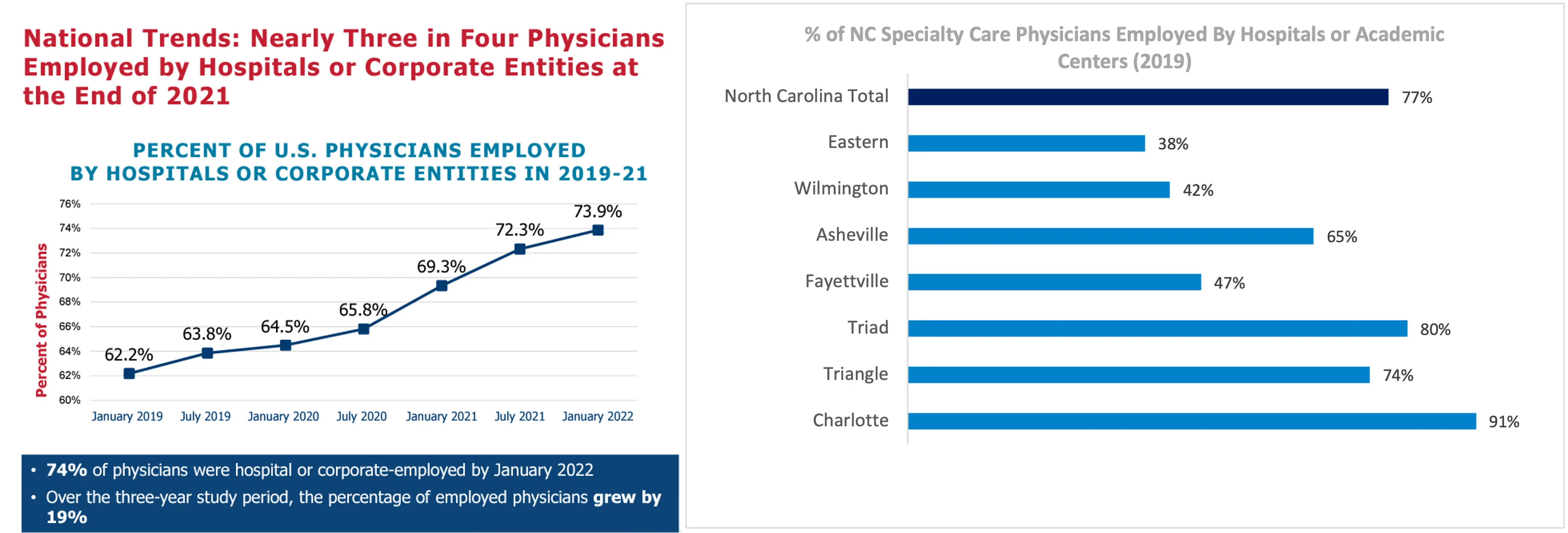
However, we all know incentives drive decisions. By definition, for-profit health plans must focus on maximizing returns for their shareholders. And given the massive consolidation ongoing, this creates an ominous sense about the future of US health care system, when considering the following:
- Optum is now the number one employer of providers in this country.
- Across national payers, most have either an acquisition or a deep partnership across every part of the value chain in healthcare (specialty pharmacy, pharmacy distribution, retail pharmacy, pre acute care, post-acute care, BH, infusion and digital/virtual health).
- In theory, when you think about the equation for MLR, owning both sides of the equation (and all the pieces in between) could lend itself to actually drive-up overall prices
I am not saying all this to knock for-profit insurance; their scale allows them to bring needed innovation and efficiency (that places a ton of competitive of pressure on us, that we would not perform as well without), but I am saying when you follow the money, you often learn a lot about what is driving decision-making.
Nonprofit hospitals have a special tax status, which has a big impact on the amount and use of revenue. At Blue Cross NC, while we are a nonprofit, we are fully taxed — state and federal.
Hospitals, generally, as well as specifically in NC, are creating significant consolidation. In NC, the top 5 health systems now own 63% of the beds, up 13% from 2019 and the literature on the upwards pressure that this causes on pricing is well documented.
Nonprofit Payer Difference: As a fully taxed nonprofit, we don’t answer to investors or financial shareholders pushing for more revenue and profits. Our community views us as an entity there to serve the state, and our regulators that govern us hold us to this. That means we have different restrictions that are meant to help ensure we stay focused on doing the right thing for North Carolinians. Our nonprofit status gives us the freedom to think longer-term around investing in health and gives us the latitude to:
- Focus on the health needs of our communities and statewide outcomes (not just our members),
- Have a longer time horizon for cost/benefit and quality decisions (due to our penetration in NC, we can think about investments in health with a longer-tail. This has implications for how we can make business cases, not just altruistic ones- on how we invest in drivers of health, curative/gene therapies, and preventative care), and
- Endeavor to offer the most affordable products.
Additionally, we realize that, if we want to deliver on our purpose, given these forces around consolidation in the market, doing nothing is not a viable strategy for affordability in the longer-term. This is why we established our DBG. However, we are under no illusions that we have an uphill to climb when considering our scale. Feels like a true David vs. Goliath fight.
3. You must get hit up by startups all the time (actually I know for a fact you do because I send them to you lol). What should a startup have ready before they approach you all at Blue Cross NC? What will get you excited about a pitch?
If you can’t help Blue Cross NC move the needle on healthcare’s affordability crisis - particularly for our neediest members- it’s unlikely you will be our focus. We all know there are a myriad of critical needs in healthcare (e.g. experience, lack of information-sharing) that payers sit at the center of, so we are accountable for working with others in the ecosystem to fix this. However, knowing that there is much to improve, and we can’t do it all at once, it’s important to remember that improving affordability to increase access and outcomes is our top priority.
This means a lot of things that are really important can still not make the cut. One extreme example that stuck with me when learning this rather painful lesson is back in my pharma consulting days. We were seeing a drug that potentially cured blindness (wow, science!) being worth significantly less from a cost-effectiveness stand-point (note cost effectiveness is the methodology used in several countries, including the UK, to determine prices paid for drugs) than something that would potentially improve hospitalization in a chronic disease.
At the end of the day, insurance is incentivized to help lower the cost you are paying for care, but this is not tied to all things that will maximize your wellbeing holistically. And understanding the tension between needing to keep our products priced affordably and wanting to cover other things that will make your life better, is a very important piece many folks forget when talking to payers. It's not that I don’t want to cover your new solution, but the reality is that it may drive up costs in an already unaffordable system.
In terms of what gets me excited about a pitch, it's when innovators can make an impact without needing to integrate with our core systems. That allows us to achieve quick wins without me needing to fight for funding or capacity resources which slows us down and often becomes serious roadblocks. An example of a meaningful, but quick win was establishing our collaboration with Turquoise (thanks for sharing them with your readership, Nikhil!), who was able to help us save meaningfully on our network contracts ($$$) without requiring any integration with the business.

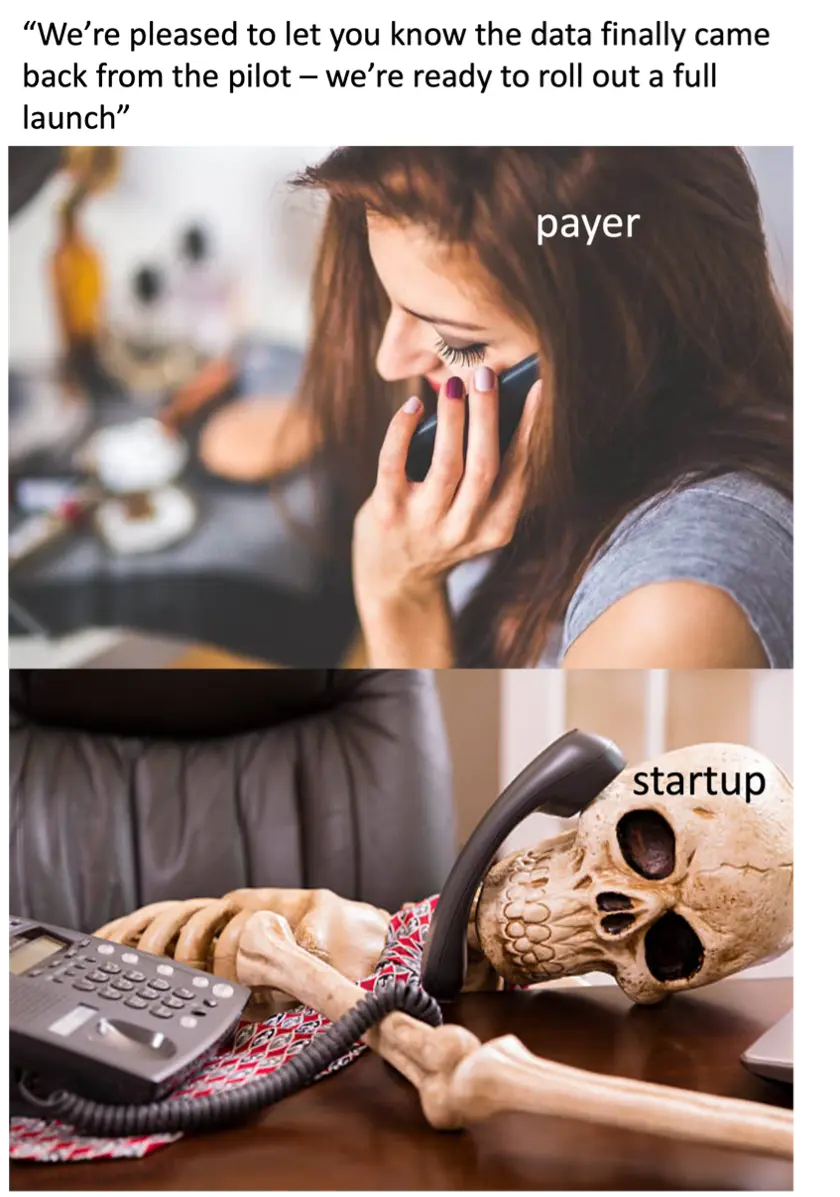
4. How do you structure a pilot with a startup? How do you think about metrics of success for the pilot, payment, and figuring out how to work together post pilot? What goes into the best/worst pilots you’ve seen?
For our strategically important areas, we tend to prefer being an anchor customer. This means Blue Cross NC would be an early customer who is essentially co-developing your solution alongside you with the help of our internal subject matter experts (as a plan who has been an early adopter of innovation, there are many examples of this: Cityblock, Aledade, Eleanor, Headway, Carrot, Strive, Galileo to just name a few).
It takes a lot of diligence and investment in resources to find the right partners – ones that align with our values. Upon finding them, we prefer to invest in a more lasting way. This approach benefits both sides because we are ensuring your solution is designed with the deepest understanding of our member communities, and that your solution will be more likely to prove out results you can point to in future selling.
In these cases, we also tend to be understanding of the fact you may need to work your way towards putting your fees at risk. Just know that with our focus on affordability and access, unless you are an employer buy-up (where employers are willing to pay more for you as a separate line item) or in some other niche of our health ecosystem where we have a need, Blue Cross NC will want to see a neutral impact on premium.
However, for areas where there isn’t that level of momentum internally (tough to get!), pilots are a great option. These come together most quickly when you can make it a “no brainer” so that your internal sponsor has minimal battles to fight. It becomes hard to say no when you can offer a meaningful solution that:
1. Requires minimal technological integration with us
2. Involves fees that are somehow tied to the value that you create.
Keep in mind that I am speaking very broadly in generalities here - when there are a lot of nuances that happen at the line of business level, for example, employer, ACA, or Medicare. Generally, solutions that do not remove some of barriers remain stuck in the “will they/won’t they” spin zone.
When thinking about metrics, there tends to be a data delay for risk-based contracts by nature of what you are measuring. For example, tracking hospitalizations over a certain period of time. While you want to measure these items, you also want to incorporate leading measures. Balancing different types of metrics in the model builds in “checks” that better validate the results.
5) As someone whose company is a big player in the shift to value-based care, what have been the challenges with making the shift?
When embarking on this push to fundamentally change how our health system works, we never expected this to be easy, and we know there is still a journey ahead. However, the numbers don’t lie, and at Blue Cross NC, we have seen that value-based care works in terms of improving cost and quality. However, it is important to remember that based on our unique market position, we have been able to approach this in a way that might not be replicable to others. As shown in the paper after paper on value-based care with slightly disheartening results, the devil is in the details with how you design the models and being the market leader in our region allows us to have more authorship over those details as well as develop deeper partnerships with the systems in our state to build out new models of care.

Interestingly, as a whole, COVID-19 created tailwinds around value-based care as our providers pushed toward value-based care as they sought greater economic stability.
One of our greatest successes around this has been continuing to empower our primary care physicians. An example of this is the Managed Services Organization, Alo, we established with Deerfield to help keep primary care practices afloat. Alo provides scaled capabilities (e.g. Rev cycle management) to independents to help keep them independent and protect affordability of networks in our state.
However, moving forward, we are all going to need to continue to solve for a number of challenges to continue the push in the right direction, including:
- Economy: Looking ahead, strong inflationary pressures might materially increase healthcare costs, including double-digit provider rate increase requests.
- Value based care: Continuing to embrace value-based care as not just a payment model but also a partnership between payers and providers to think and work differently together.
- Consumerism: Expectations across industries have been rising – and healthcare is no exception. While these trends are impacting the entire HC industry, NC has been a leader in innovation in healthcare, placing unique pressure on Blue Cross NC to deliver better, faster. Consumers are increasingly optimizing health care choices; our data shows 33% of consumers are considering switching plans due primarily to affordability and benefit coverage reasons.
6) Which segment (Medicare,Medicaid, Commercial, etc.) are you most excited about going forward and why?
While, I am excited about Government blazing the trails when it comes to value based care and incorporating drivers of health and health equity, Blues have strong local power in their respective commercial markets that allow for market-making when it comes to value-based care and more creativity for consumer-based models.
As I noted, Government segments are pushing for some meaningful changes to our healthcare system. COVID-19 cast light on behavioral health, racial and poverty inequity crises facing us in U.S. health care, and we saw a quick and thoughtful— though most definitively not holistic — response. Payers changed payment models and federal/state governments issued sweeping regulatory waivers and rule changes. As a collective, we made meaningful strides to build more equitable systems during the pandemic, and I am energized in particular for the government segments to harness the power of that momentum.
However, from a local Blue perspective, I am more focused on Commercial because at this moment it’s where we have more autonomy and ability to think a bit differently. Commercial segments, while still shackled with the perverseness that is the US healthcare system, in general run more closely to our broader free market economy. This means that as a Commercial insurer, it’s your job to figure out how to bring quality products to market more cheaply -and it’s up to you to figure out how to get there.
Zeroing in on the consumer-based models, we have seen a number of exciting models emerge including: new takes on the reference based pricing such as Sidecar (although these can still leave members on the hook for large, unexpected bills), advanced primary care built in at $0 cost share to products like Poppins, and employer direct contracting, like what Blue Cross NC owned Brighton and Northwell Direct have embarked upon, which in many ways is the ultimate realization of value based care and meaningfully limits the legacy payer’s role (yes I mean us - and we are comfortable with that 😊) to lower cost. We are only at the beginnings of harnessing technology and data to connect members with the right care at the right time- and employers are the incubators for these models.
7) Is there a startup or solution you've been looking for that you just haven't seen yet? What's a pain point you all feel that you wish someone would build for?
One of the areas that I have spent a lot of time thinking about is disruption in pharmacy. Pharmacy costs now make up ~1/3 of our total medical spend, and this is increasing every year. As a relatively small player who doesn’t own the dollars of the other side of pharmacy - entrenched, large players make this an area that in many ways we are quite frankly are out of control of. For example, if a drug costs $100k per year, you are paying $5k and we’re trying to not make up the difference by charging an absurd amount on your premium.
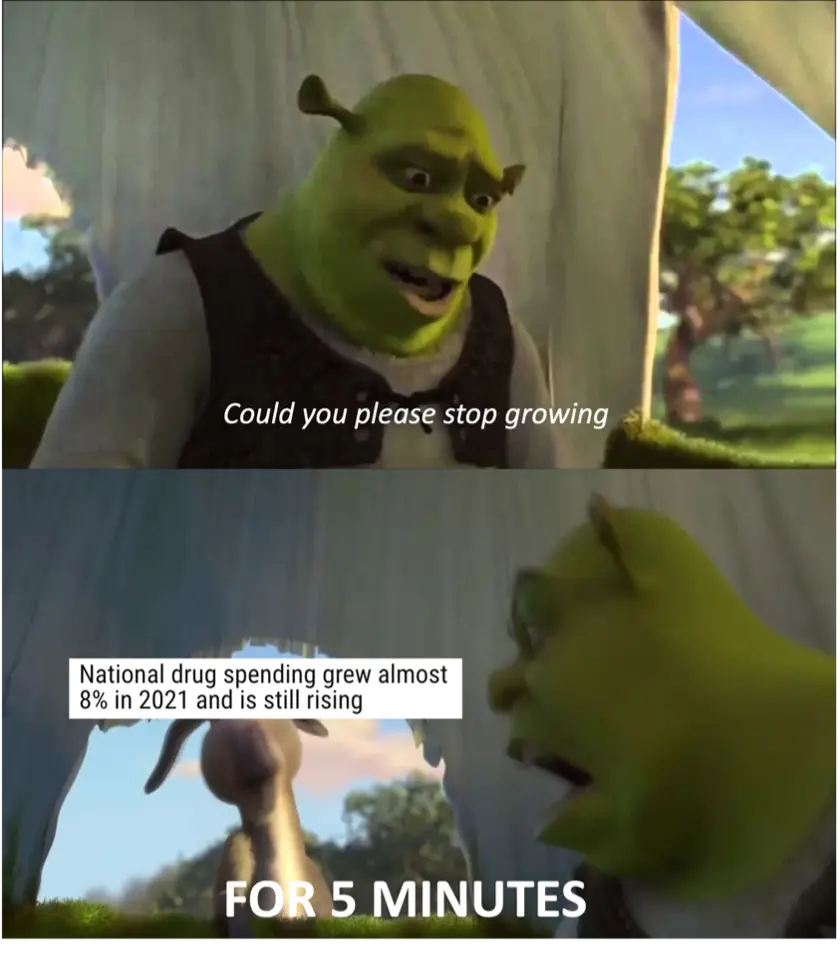
There are several interesting models that have popped up: CivicaRx and EQRx (who I personally structured a BlueCross NC partnership with) where payer direct-to-manufacturer relationships have demonstrated very meaningful ways to reduce cost, but there isn’t a scalable way for smaller players like us to support this. A player to help with the contracting, distribution and outcomes that has different incentives than the traditional PBM model could help make more of these models emerge and even disrupt areas with meaningful gross to net bubbles (IYKYK) that have been historically difficult to make meaningful impact on. Reach out if you want to talk thoughts!
8) How do the Blues interact with each other? Are they totally separate, or are there shared learnings and infrastructure?
The BlueCross Blue Shield Association is an association of independent, locally operated Blue Cross and Blue Shield companies, including Blue Cross NC.
Most Blues (there is nuance based on corporate structure) have a similar local and mission focus. They also have a lot of shared challenges by being the “David’s” in this Goliath competitive environment. Because of this, Blues have worked to build out shared infrastructure and knowledge-sharing through the Association as great “phone-a-friends” for shared challenges.
Interestingly, one of the best models I have seen to facilitate collaboration amongst the Blues actually comes from start-ups and disruptive companies that become “Blue utilities”, which are companies that focus on the Blues’ shared challenges are usually able to assemble several Blues flagship customers and build momentum from there.
Beyond this, we do have shared infrastructure, including: Blue Health Intelligence as a shared data repository; and our shared fund investments, such as Echo Health Ventures and Blue Venture Fund, serve as a collaboration and co-investment channel for several other Blues.

While outlined some successes above, we need to see more examples of collaboration amongst the Blues in areas that require scale in the future because I think this is necessary for them to continue to be around for the long-term.
Bonus: I know you’re a die-hard true blue North Carolinian. What’s the biggest beef for North Carolinians that isn’t Duke vs. UNC?
The classic one would be vinegar vs. tomato based bbq sauce (seriously, politicians who were clearly focused on the most important issues 😉 tried to pass bills on this), but I think the real one is: what is the top reason NC is such a great place to live- could it be access to topnotch beaches and mountains, or is the low cost of living paired with being ranked as CNBC’s top place to do business this year? Thanks for teeing me up for a shameless plug to recruit your smart readership to NC (and potentially to Blue Cross NC) 😊.
Nikhil aka. "peter piper picked a payer pilot"
Twitter: @nikillinit
Other posts: outofpocket.health/posts
{{sub-form}}
---
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







