Should we charge for patient messaging?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
New Discussion Post
Today I have a new post and discussion topic.
To reiterate the rules:
I’ll pose a question and give my thoughts. In a future newsletter I’ll include ~3 of my favorite answers people reply with. I’ll possibly even make a meme related to your answer.
Good answers are ones with a novel viewpoint, data to back up their claim, personal stories, and avoid clearly shilling something.
Please reply to this email with your thoughts on the question and let me know if you want to have your name included or be anonymous. You have to actually be on the newsletter to submit a reply to it obviously.
Try to keep answers to two paragraphs or less please. This obviously doesn’t apply to me because it’s my newsletter and these are house rules.
Is billing for patient messages bad?
Before COVID, I think I maybe logged into my electronic medical record once. This was mostly for inspiration since I was trying to design an escape room.
During COVID, however, test results were being released through MyChart (Epic’s patient portal) so I was looking at it a bit more often and it became a more regular habit. This is also when I discovered that you can message doctors through MyChart after you saw them and they’d respond.
It turns out during COVID a lot of people discovered that same thing. MyChart messages have ballooned in the last 3 years and the time spent in EHRs to handle these requests has increased as a result (this paper is good and looks at this phenomenon).
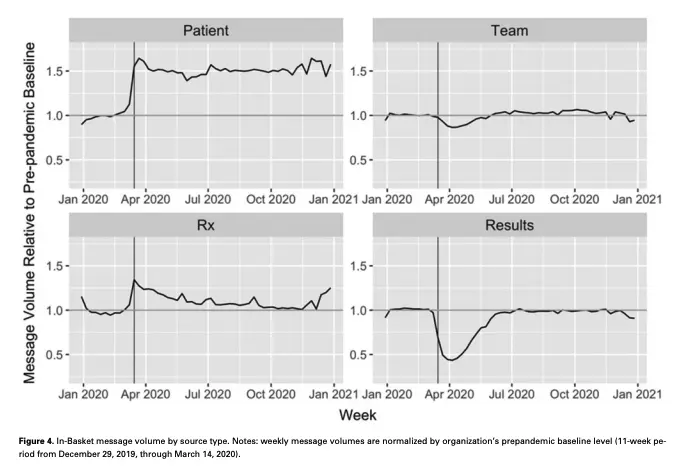
So, hospitals did what any non-profit would do…start charging people for that pleasure. Thanks to some new CPT codes (99421-99423), providers can charge for messages initiated by patients that require some level of complexity. In 2023, several health systems began implementing this including Mayo Clinic, Johns Hopkins, etc.

I’m getting flashbacks to 2005 pre-unlimited texting, wondering if my parents are going to tear me a new one when the text bill comes in.
So my question today is…
What’re your thoughts around the new push to bill for patient messaging?
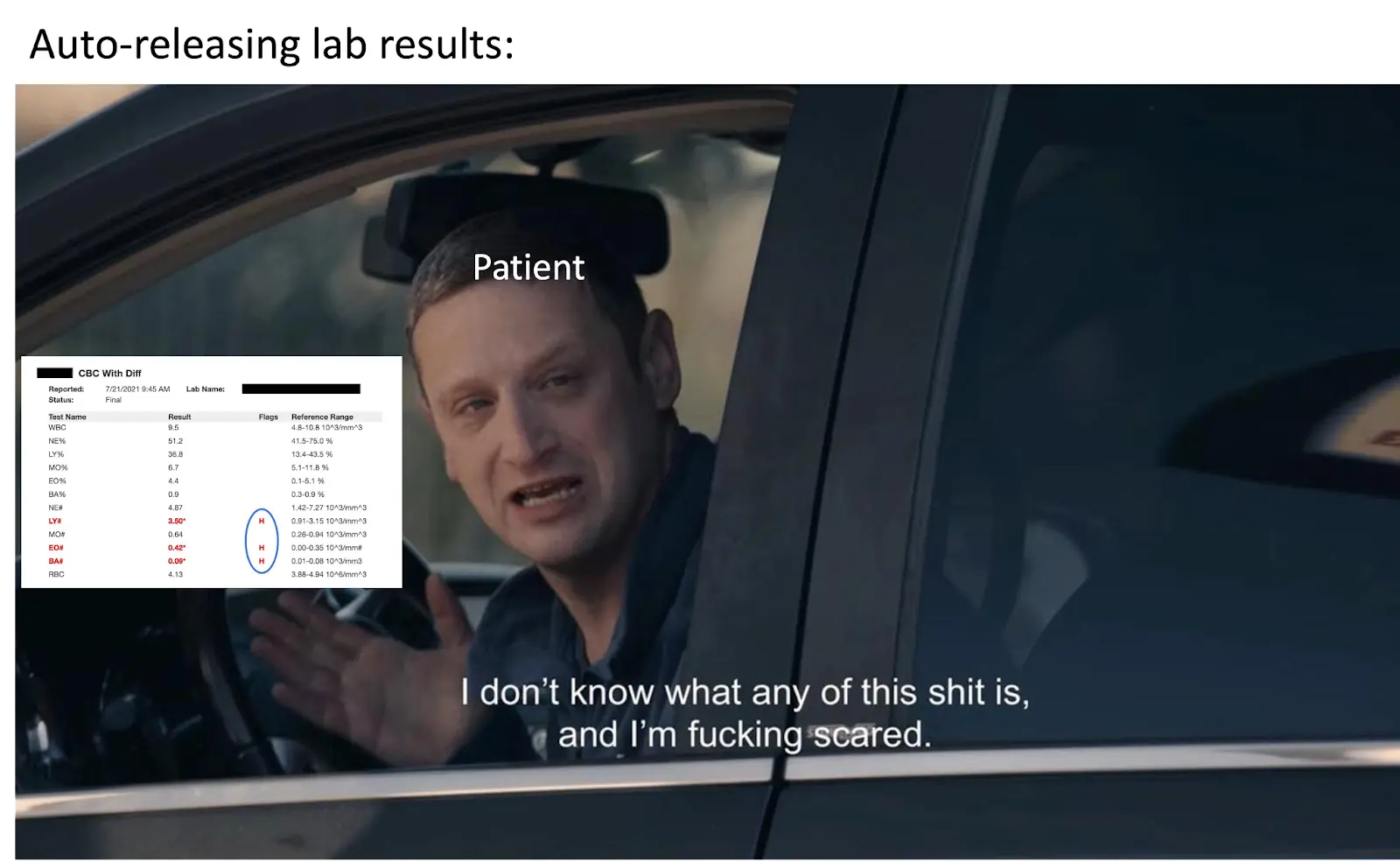
I’m sympathetic to doctors and hospitals here. I’m imagining a world where I had to respond to each email I get quickly and empathetically or I’d get yelled at. But instead of someone emailing “hey mind looking at a draft of this post also I’m publishing tomorrow and not making any changes”, it’s “hey I got these lab results back and Google says I’m dying?”.
Responding to messages, especially in ways that make patients feel heard, is hard and also requires expertise. I actually think it makes sense that they’d want to get compensated for the time they spend on these messages - if the patient is asking something complicated then why should it be different if they answer that question via message vs. in-person?
Many other service industries are similar. I’m fairly certain that each time my lawyer ends their message with “Regards,” my bill goes up $0.05 and I start idly wondering if I’d get jail time if I didn’t use them.
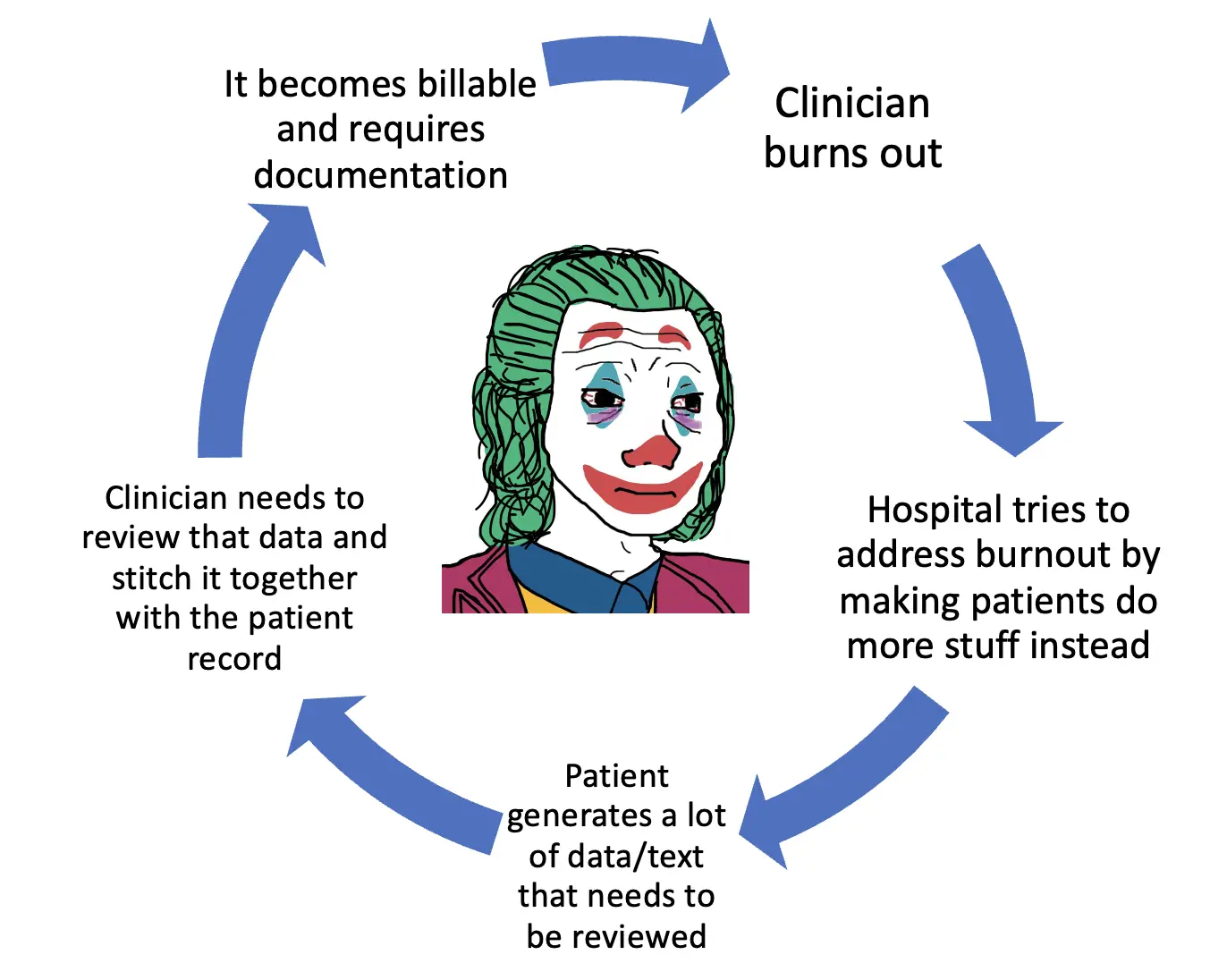
It’s inevitable that lowering the friction for reaching your physician is going to increase the amount of patients that demand their attention. But I think how we’re thinking about charging for this service represents a lot of things wrong with healthcare:
- The CPT code parameters seem silly. They change based on the amount of time spent on the message, and if it’s at least 5 minutes, it’s billable. That’s obviously going to be gamed by providers and is paying for time spent instead of expertise. I’d rather the best oncologist in the world bang out a bunch of 30 second messages and get paid well for seeing lots of people. Plus you can only bill that code once per week…what if a patient has complex questions more than once per week? If you’re going through an acute episode, that might be likely.
- Most institutions charging for these messages seem to be large academic medical centers where the docs are largely salaried, so it’s not REALLY like they’re getting directly compensated for doing this. Which begs the question of what the goal of charging patients is here? To give physicians money for their time (unlikely), a gating mechanism so less messages come in (probably), to compensate hospitals for the opportunity cost of other missed fee-for-service visits (more probably), or for the hospital to get money from something docs are doing anyway (definitely)?
- Patient messaging presents a great opportunity to build a longitudinal relationship and trust, which is sorely lacking. I quite literally only trust the homies that text me semi-regularly with memes and questions about our role in the universe whether their doctor is in-network. I’m genuinely excited when the groupchat gets an alert. Modern relationships are built on text, which should include our relationship with clinical teams. If a patient is willing to go through the Sphinx-style riddle that is logging into their EMR just to message you, they’re doing it because they need help and trust the clinician to help. But clinicians already now have a negative pavlovian response to seeing inbox notifications as Ajay points out in this thread. By introducing billing, patients end up messaging less (source).
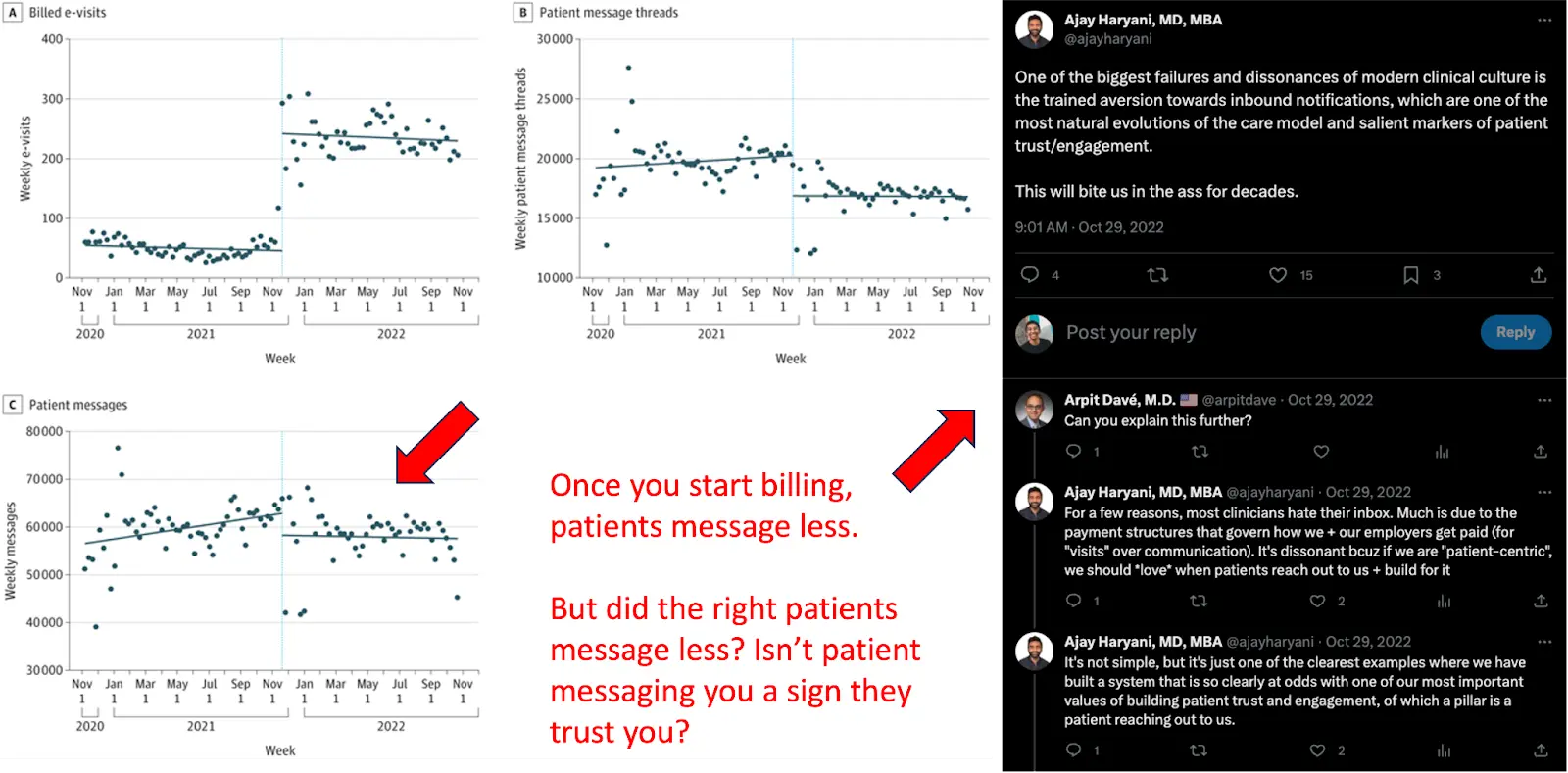
- The people that will hurt the most from this are people that require the most help but are least able to now pay the co-pays for these visits. Some hospitals are making it no-pay or discounted for Medicaid/Medicare patients. Others are charging $7-28 for Medicaid or higher for totally uninsured.
- The notifications are absolutely fucking useless. I get emails at least once a month that’s like “you have a message in your MyChart” and my heart skips a beat wondering what’s wrong. Ah nvm, it’s simply a reminder to get my flu shot. Everytime this happens I want to find the person in charge of hitting patient engagement metrics and engage their face with my foot. I can’t imagine how much worse this is on the physician side.
As a whole, I don’t think it’s crazy that physicians are now billing for their time handling messages. I just think the implementation of it kind of sucks.
Inbox triaging, value-based care flows, and vulnerability
The real problem this boils down to is triaging the inbox. Some requests are for a prescription refill, some are patients trying to understand their lab results, some are patients trying to get diagnosed, some are substack newsletter you never signed up for. Theoretically, hospitals have systems where medical assistants/nurses do some of the triaging, but if you talk to any clinician, they’ll tell you that it’s a very janky workaround and almost always results in the doc looking at most of the message anyway.
Now that you can bill for certain types of messages, I actually wonder if this is an incentive for hospitals to set up better systems for triaging to quickly get low level tasks on nearly auto-approve status, leaving just the billing tasks for the docs. Or if they just know the docs will respond anyway and they’ll do it during their off hours.
I’d guess that the entire existing workflow and tech stack will make it near impossible to do proper triaging in any big hospitals built around fee-for-service billing. The natural response would be “value-based care solves this”. Give a company a fixed fee per person and they’ll actively push people to asynchronous messaging, manage the inbox with a team, and use software to prioritize which messages to get back to based on the patient history and content of the message.
But I’d be curious to hear from clinicians who have made that transition from a fee-for-service provider to a value-based care one if the inbox problem is actually better?
My hunch is that software isn’t good enough to do a good job of triaging messages as they come in and there’s still a clinical person mostly triaging. But software probably is good at triaging the patients themselves and figuring out which ones to start an async message conversation. It’s more about building a totally different care model involving proactively reaching out to patients, which results in very different messaging flows.
Or the patient panels for these value-based care companies are just so much smaller than what a hospital typically has to deal with, and if they grew, they’d have the same issues.
But maybe all of this is actually more solvable with good old honest communication instead of business model shenanigans. Probably one of the best pieces I’ve read about this is a firsthand account of someone drowning in their inbox and then setting rules for patients on engagement:
“After several desperate weeks, I decided to send a portal message to my entire panel of patients. I was uncertain how they would respond. In this letter, I confessed to feeling burned out, expressed my desire to continue to provide attentive care, then laid out several guidelines for portal use. The first was that I was going to stay off the EHR on weekends, and that if there was an emergency, telephone coverage with an on-call physician was always available. The second was that my office staff would begin to handle some messages, so that I, myself, may not respond to all questions and requests. The third was a plea not to send frivolous messages and, if possible, to save less urgent concerns for the next appointment. The fourth was to see me in person to address complex medical concerns, and not to relay them via the portal. This not only would reduce my EHR use but also would help ensure that patients were getting the appropriate evaluations they deserve…
Within a few hours of sending that message, I received more than 50 responses from patients (all with apologies for using the portal) assuring me that my requests were reasonable and that they would help take care of me as I had of them.” - Michael Stillman MD, JAMA
If we had longitudinal relationships with a doctor and they set those rules in place, I think I’d have a better understanding on how to engage them through messaging because right now it’s totally unclear. I don’t want my doctor burnt out either, I can hold off on sending a 50 page PubMed article with the title “Thoughts?” and nothing else.
Anecdotally, direct primary care docs seem to do a good job of setting these boundaries around when they’ll be able to respond and what’s appropriate to message them about. That’s something you can do when you know you’re going to have a longer relationship with a patient.
Maybe we don’t need to overcomplicate this problem with new incentives and billing structures or technology. It’s really a person-to-person communication problem.
…you thought lmaoooo, let’s talk about GPT.
Large Language Models and the Inbox
The obvious question to ask is…do large language models and chatGPT eventually help with this problem? You can see some experiments here at the edges. UCSD is piloting a chatbot in patient-doctor messaging where the doc can approve a bot-generated message (and the patient gets notified it’s bot generated). UNC is testing out something similar. Epic and Microsoft are partnering on using GPT for inbox responses live in a few sites already. And lots of people have been messing around chatGPT to respond to common patient inbox messages in a janky, workaround, non-integrated workflow.
This was a great post from Karl Swanson where he created a bunch of different inbox message types and showed that the bot performed really well for things like medication, questions, diagnoses, and follow-up if it had the full context of the patient. Without it, the bot tends to make stuff up. So I’m pretty optimistic that bots either trained on local clinical data + the patient record or data from the EHR generally will actually perform as well as physicians for routine stuff soon. With interoperability rules theoretically around the corner, maybe we can authorize a bot with our data to just tell us what we want to know.

It seems like eventually it’ll go something like “bot generated -> MA or nurse approved -> physician signed off” and eventually just become a physician sign off.
HOWEVER…here's a thought experiment. I think it would be interesting if patients could opt-in to getting an immediate response from a bot if they wanted. Imagine they were given the information on how accurate the bot was at certain types of requests + how long it would take for the doctor to get back to them if they waited.
Every physician would train and give a stamp of approval to a trained bot based on the physician’s style, how they like to respond to certain messages, etc. The physician would take the malpractice risk of a bot (essentially using a collaborative practice agreement with the bot). Patients would choose to opt-in to a bot response and the physician could charge differently between a direct visit with them vs. their trained bot response. The patient gets faster responses and a bot they could keep asking follow up questions to, and the physician can theoretically manage a larger patient panel.
Large language models aren’t quite there yet, but it seems like they aren’t far off either. Maybe the next large-scale reinforcement experiment to train AI will be patients and docs reacting to auto-generated mychart responses to train individual models. Then you can see Dr. OzBot for cheap if you want!
Conclusion
I got pretty derailed, but let me know what you think about this whole “charging for patient messages phenomenon” that’s happening. Or if you want to shit on my thought experiment, I’m always happy when that happens (not in a kinky way).
This feels like a pretty recurring phenomenon that isn’t super new (prior examples include remote patient monitoring, chart review, etc.), so it’s probably worth talking about as a group.
Nikhil aka. “is it just me…is it just me…or are these texts so good I shouldn’t have to message for free?”
Twitter: @nikillinit
Other posts: outofpocket.health/posts
P.S. Claims Data 101 course starts in a couple weeks - it's a must if you're someone that deals with claims or analyzes claims data. Sign up here.
{{sub-form}}
--
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







