The Upfront Pricing Phenomenon
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
I distinctly remember someone once telling me that they hadn’t gone to a primary care physician in years because they didn’t know how much it was going to cost. Not that they knew and couldn’t afford it - they actually didn’t know. In fact…it was actually included in the premiums they were already paying!
I wonder how unique that person is, or if a lot of people avoid care because they’re scared of getting hit with a random bill 90+ days later that they don’t understand. My guess is that it’s not an insignificant number. A questionably formatted TransUnion report found:
…62% of respondents said knowing their out-of-pocket expenses in advance of service impacts the likelihood of pursuing care. Furthermore, nearly half (49%) of those surveyed said having clear information on expected out-of-pocket costs before receiving treatment impacts their decision to use a healthcare provider.
This is bad for everyone: avoiding care means hospitals don’t get paid, patients are potentially getting sicker, and insurers will end up paying for more serious diseases that weren’t caught earlier.
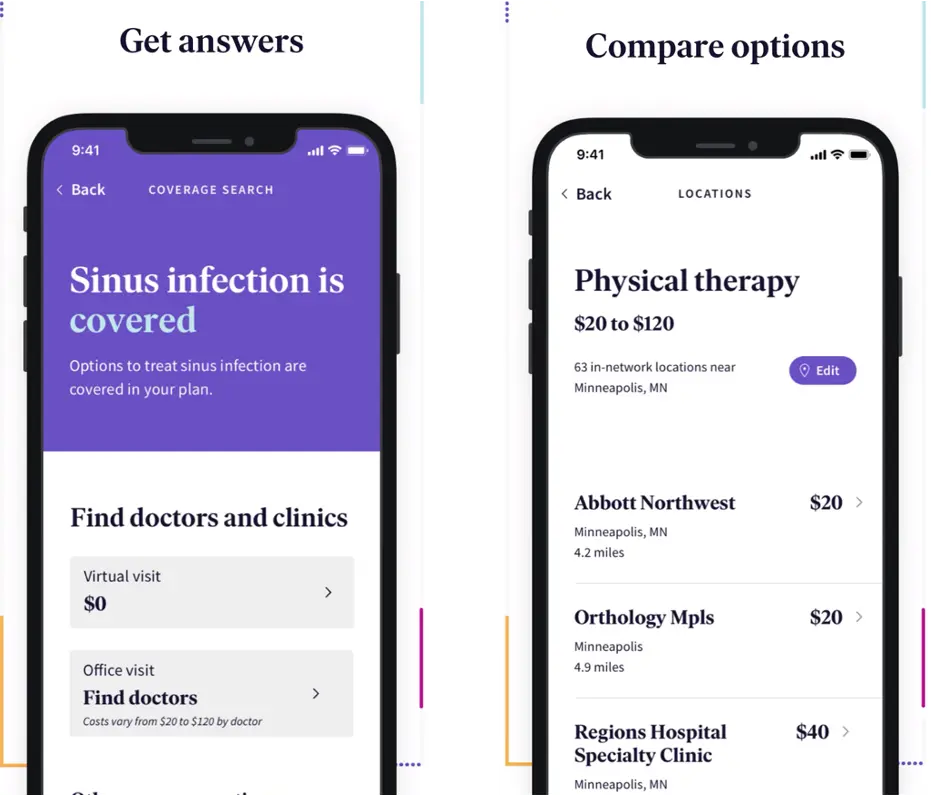
Interestingly, there seems to be a wave happening where companies are focusing specifically on making prices fixed and transparent for a very specific episode of care. Some examples:
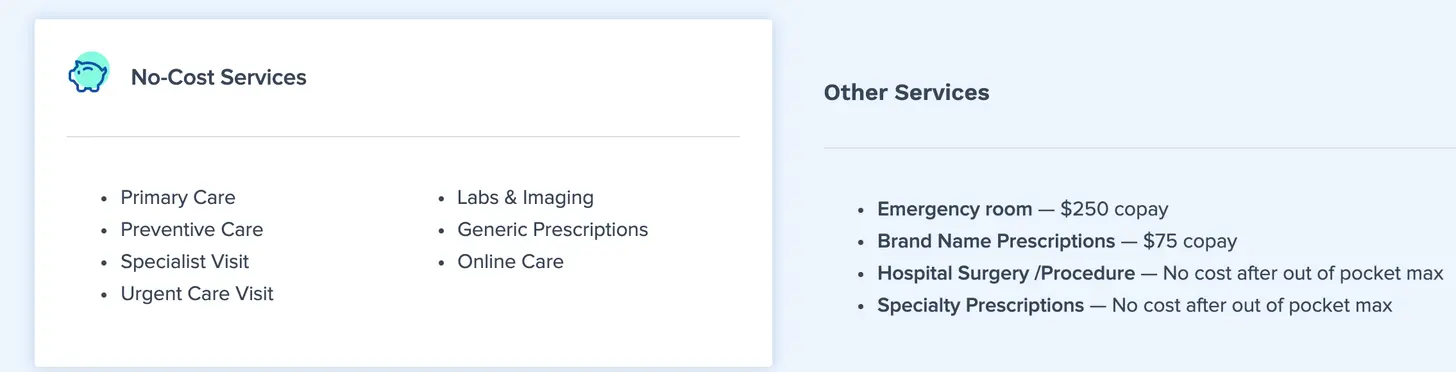
- Oscar offers $0 virtual primary care visits with many of the follow-up services (labs, imaging, etc.) needed also being $0
- Gravie Comfort offers specific upfront costs for different tiers of services
- Direct primary care offers cash pay visits that you know the cost upfront for the entire visit upfront. For example, this doctor charges a flat $35 per visit.
- Direct-to-consumer cash pay pharmacy companies like Ro, Hims, etc. are clear and upfront how much a visit + medications are going to cost.
- Bind Health is insurance (for self-funded plans) that removes coinsurance and deductibles, and instead gives a specific amount to you upfront that you’ll pay for a bundle of services at a given facility.
The goal here is to make it less confusing for patients to get care by making it clear how much they’re paying in advance - and I believe it’s a result of a few trends.
- Cash pay patients are on the rise
- Deductibles are weird
- The bet on patients being good shoppers for their healthcare has failed
- Ability to use data to better predict exact costs and how much follow up care you’ll need
Cash pay patients are on the rise
Patients in high deductible plans are not true shoppers since their insurers are negotiating prices on their behalf. TRUE healthcare shoppers are the uninsured that are paying cash pay prices. This was already ticking back up pre-COVID, but now the uninsured have spiked to somewhere between 15-20% of the non-elderly population (though this may have decreased with some of the Medicaid expansion that’s been happening).
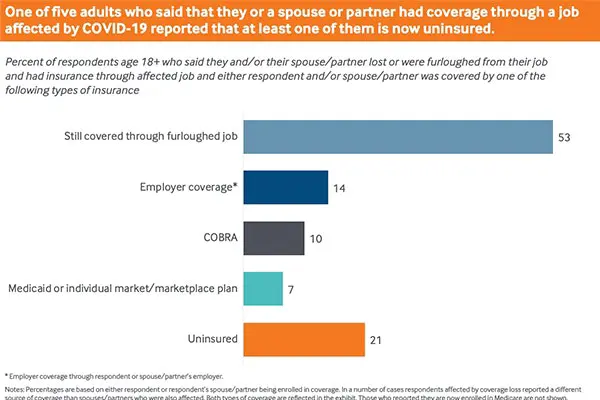
As this segment increases, more viable business models NATIVE to the cash pay population can be built. The reason they have to be native to this population is because frequently the list or cash price is used in some capacity during negotiations with payers, PBMs, etc. The list/cash price might be an anchor price (e.g. we’ll pay X% of your usual price) or it might act as a ceiling (e.g. we’ll pay $X or the list price, whichever is lower). Plus, having the billing admin + infrastructure required to take insurance isn’t cheap and will creep into your prices.
So because of that, if you build specifically for the cash population you can be very clear and upfront about your pricing (especially important since this population will be most worried about unexpected charges and also least likely to pay them).
Deductibles are weird
When you think about what a deductible is, it’s pretty weird. It’s the amount you have to pay before your insurance kicks in, so theoretically you’ll be more price sensitive below that amount. But here’s the issue:
- Deductibles reset each year. So if you hit your deductible in January because of an operation or something, you actually have an incentive to use MORE healthcare through the rest of the year. If you haven’t hit your deductible in December, you’re incentivized to push off potentially necessary care to January.

- Because of the yearly deductible, we’re forced to guess how much healthcare we’re going to use in a given year. This is basically impossible except people that know they’re going to hit their deductible because of an operation or because they have an expensive chronic disease. Healthcare spend for everyone else is totally unpredictable, where you might spend $0 or the entire deductible (sometimes $5K+).
- The deductible is the same regardless of the type of visit you have. If you have an $8,000 deductible (whatup Oscar Catastrophic), that’s terrible if you’re only getting preventive health visits but fantastic if you end up in the emergency department.
- Despite the fact that you’re price sensitive below the deductible, you can’t actually negotiate any of the prices yourself; if you want it to apply to the deductible, you have to use whatever rates and network your insurance has negotiated for you.
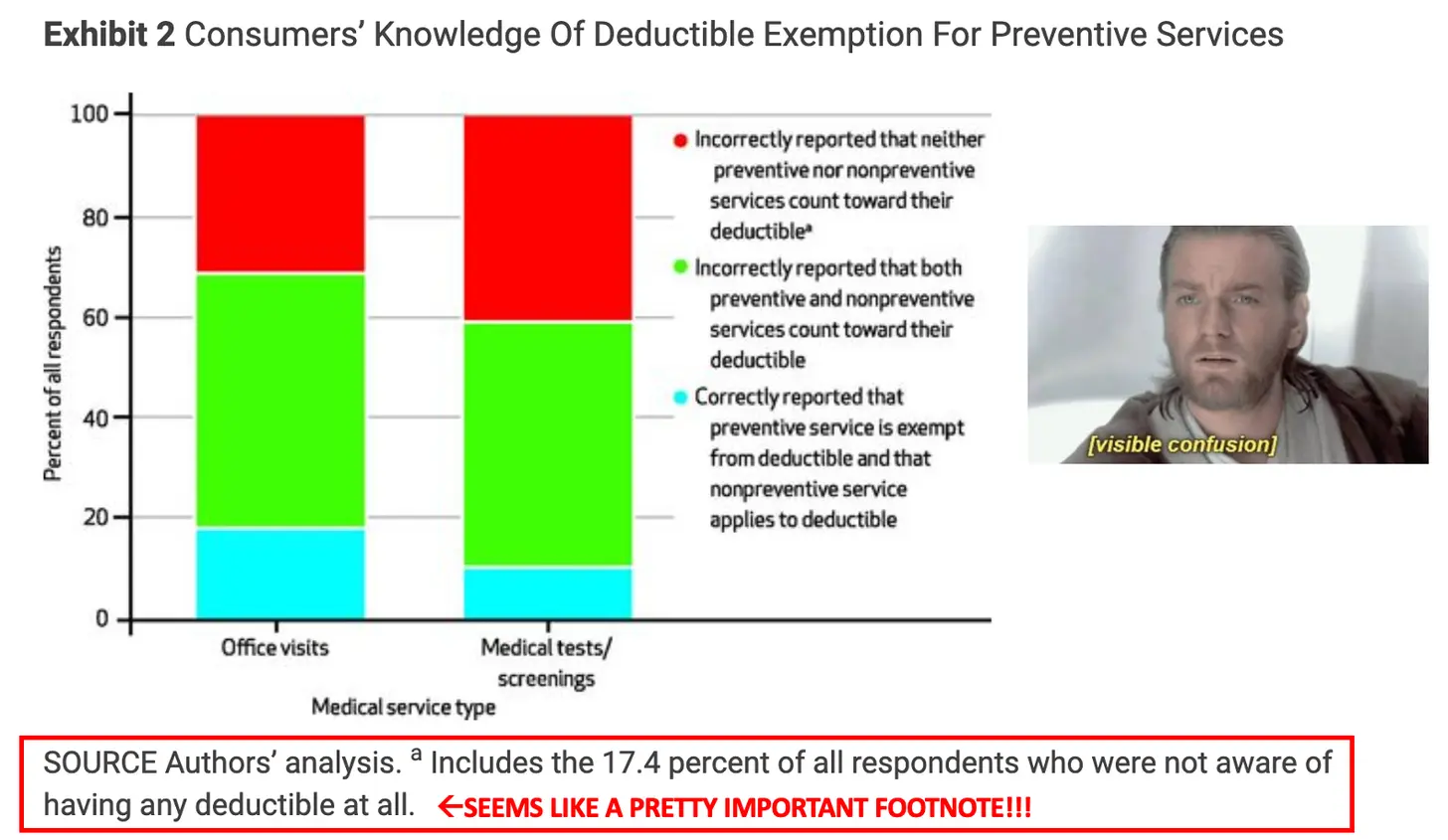
Because of this, people are now trying to guess if it makes more sense to pay in cash, which might be cheaper vs. their insurance rates, but won’t count towards the deductible. Also patients are putting off preventive care due to cost, which is defeating the purpose. Deductibles have become confusing for most people - studies show most people don’t even understand what actually counts towards their deductible or what’s covered for free. Plus, deductibles are now so high that they effectively only act as insurance against catastrophes.
Companies have seen this as an opportunity to sell predictability, which naturally includes upfront pricing. Some examples:
- Enroll in a monthly direct primary care subscription that covers everything except true unplanned catastrophes like cancer via catastrophic health coverage a la Decent, or stop loss insurance for an employer.
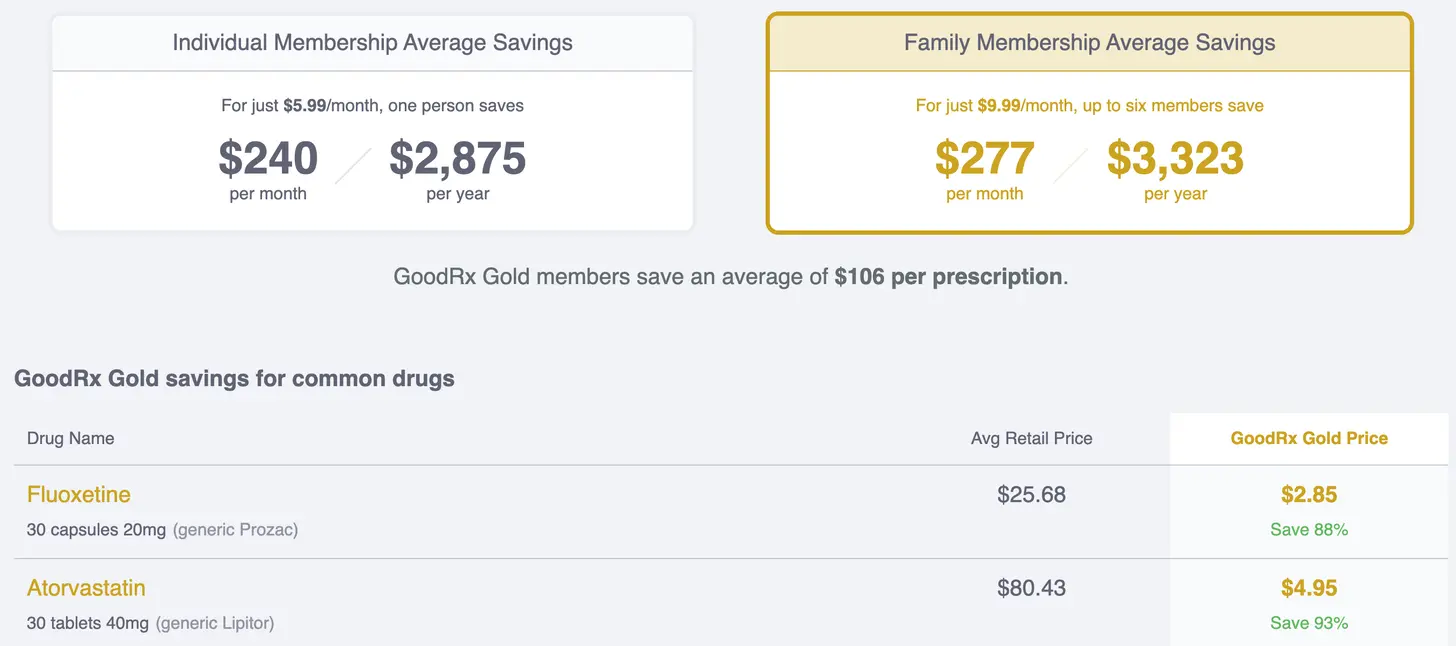
- GoodRx Gold monthly subscription for patients with predictable medication costs that won’t actually meet their deductible. If you’re on the list of generics, you know exactly what you’ll pay each month.
- Bind Health removes deductibles and creates two tiers of coverage - preventive visits which are included in your premiums and then additional coverage for planned procedures that you purchase upfront before the procedure.
- I can bet Walmart Plus will eventually include a layer of preventive health services from its primary care centers + prescription drug list within a tier of its subscription.
There’s a wave of products that have figured out what bundle of preventive/recurring care they can sell for a monthly price that people will pay for just for simplicity and peace of mind. Plus in a scenario where something unexpected and extremely costly happens, you’ll still have your high deductible plan and will probably meet the deductible in that one episode.
Patients Are Bad Shoppers
The prevailing theory behind high deductible plans has been that patients who have more “skin in the game” would actually be more price sensitive and shop around for their care.
I think we can say relatively definitively that this didn’t work. There are lots of studies around this, but my favorite is this one that found that patients would actually drive past six cheaper MRI locations on the way to the one their doctor recommended. If they had stopped, would have saved them more that 35% of the cost on average.
There are lots of prevailing theories around this, but in general it’s probably some combination of:
1) Patients actually don’t know when care or tests are necessary and when they’re commodities, so it’s hard for them to shop without that knowledge.
2) There’s no real means for them to negotiate, since insurers are the ones who negotiate prices on their behalf.
3) There’s a lot of weird math you have to do to figure out how much you’re actually paying once you calculate copay/coinsurance, deductibles, secondary insurance AND you have to guess how much healthcare you’re going to use for the rest of the year to actually make those calculations.
4) IMO probably most important is that patients expect their physicians to make the best decisions for them. Even in that paper earlier, that was the biggest factor.
Ultimately, we find that the factor that appears to limit patients’ ability to price shop is a factor underdiscussed in the price transparency literature. In our analysis of variation in patients’ MRI prices, we find that referring physicians heavily influence where patients receive care. Looking across the nation, referring physician fixed effects explain 51 percent of the variance (92.1 percent of explained variance) in the price of MRI scans that patients receive.

Since it’s clear that patients aren’t great shoppers themselves and it’s everything after the primary care/first specialist visit that’s costly anyway, more payer entities are realizing it’s actually just better to just give the initial visit away for free. That way patients are more likely to go where it’s free and then those doctors can refer the downstream commodity stuff (labs, diagnostics, etc. where there’s a ton of price variance) to the most cost-effective place.
Plus, since fewer and fewer patients have a primary care physician, an easy way to guide their choice is by saying “it’s 100% free if you go to this one”. A payer will save more giving everything in those initial visits away for free since downstream care has such a high price variance now.
Another facet of this is using price transparency to make physicians more aware of the costs their patients are going to face - effectively making the physician/patient a joint shopper. Previously physicians have thought about what care is ideal for a patient, largely without cost considerations. And most didn’t even know what the cost for anything is (fun game, ask a physician what the cost of any service, drug, test etc. is and see how many know).

But now that cost is actually causing patients to skip care, it has to be taken into consideration. One of the genius things GoodRx did was get physicians to fall in love with the product by looking up the transparent cash pay cost of different drugs on behalf of patients. They could then tell patients the most cost-effective options to make sure they actually took their meds. I imagine we’ll see more tools for physicians to help guide patients for downstream care (especially with new price transparency rules coming into effect).
Better Data = Better Cost Estimates
As more data from EMRs + claims becomes available and machine learning becomes better, payers and third-party administrators are getting increasingly better at guessing how much your care journey is going to cost them.
For each action you take in a care journey, there’s a set of probabilities for what the next action is going to be (and associated costs). Lets say I, a 28-year old, go see a doctor for migraines due to carrying the sins of the healthcare system on my conscience. Based on some of my demographic data, previous utilization, similar cases to me, that specific doctors prior recommendations, etc. we can slowly start painting a picture of how much this migraine journey is going to cost me. For specific things, like surgeries we shop for in advance, or routine things like colonoscopies we already have a pretty good sense of cost.
Once the payer (or whatever analytics company they work with) can map out the cost of the care journey, they can start presenting patients with a specific cost for that care. Sometimes the patients might go under or over. But if you have confidence in those cost predictions, you can do interesting things like what Bind does where they tell patients what they’ll be paying in advance depending on which provider they go to (and remove co-insurance/deductibles completely).
Another interesting byproduct of this is that PROVIDERS also want to be paid faster, so in many scenarios (e.g. smaller private practices) the physicians will be willing to take a pre-negotiated rate if it’s a pretty low variability service in exchange for being paid quickly (vs. the month or two it’ll take them to get reimbursed by insurance).
Conclusion + parting thoughts
I’m always a fan of more transparent pricing in healthcare, and I think a lot of these trends are in the right direction. I think for a long time we over-indexed on giving patients as many choices as possible and hoped they made the right ones without realizing the most important (and maybe only interpretable) metric for the majority of people is how much this is going to hit their bank accounts. Even worse, we tell them the answer to “how much” 60-90 days later in a completely uninterpretable format, something no other consumer facing industry does.
The counterargument to this I’ve heard is if a patient actually knows how much they’re going to pay, will they actually end up putting that visit off? For example, if it’s a screening visit or elective procedure and they get sticker shock, will people end up pushing it off and think to themselves “I’ll be fine”? I’m not sure, it’s definitely possible.
Separately it seems to me like there’s room for insurance products that are redesigned from the ground up to allow consumers to:
- Shop around a very small set of metrics they understand like cost, stars, etc. (which incorporate quality metrics that payers/CMS can use data to inform)
- Has direct financial impact both positively and negatively to the patient directly (bonus points, HSA bonuses, etc.)
- Separates different episodes of care to incentivize patients to shop when they should without avoiding regular care
- Allows a patient to do the shopping/negotiating instead of relying on the insurance company. Maybe you give patients something like a reference price for a given service and they try to shop below or above it (and I’m sure lots of tools will pop up to help patients make that choice).
Bind Health definitely seems like a step in this direction, but I think there’s room for more insurance models that think about consumer healthcare shopping from the ground up.

If you believe that healthcare will eventually be more consumer oriented, providing upfront costs and predictability will be a key component to that going forward.
Thinkboi out,
Nikhil aka. “I’ve gotten a procedure done in December and then a follow up in January and paid the deductible twice it sucks”
Twitter: @nikillinit
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







