Thinking beyond value-based care
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Is value-based care sentiment turning?
I posted on Twitter about how I’d been hearing that value-based care might actually be bad. Did you know you can post your absolute worst takes and say a friend said it? You get to farm that sweet engagement, and if it really goes viral you can just reveal who said it and @ your worst enemy. Win all around.
But more seriously, I actually have been having conversations with more people operating in the value-based care space and wanted to see if this was an opinion that was in my echo chamber, or something other people had thoughts about as well. So, I figured this would be a good discussion post.
My question to you is…
What’re your thoughts about value-based care? How have they changed over time? Are there specific slices of healthcare or value-based care programs where you think it’s working or definitely isn’t?
Some high-level value-based care thoughts
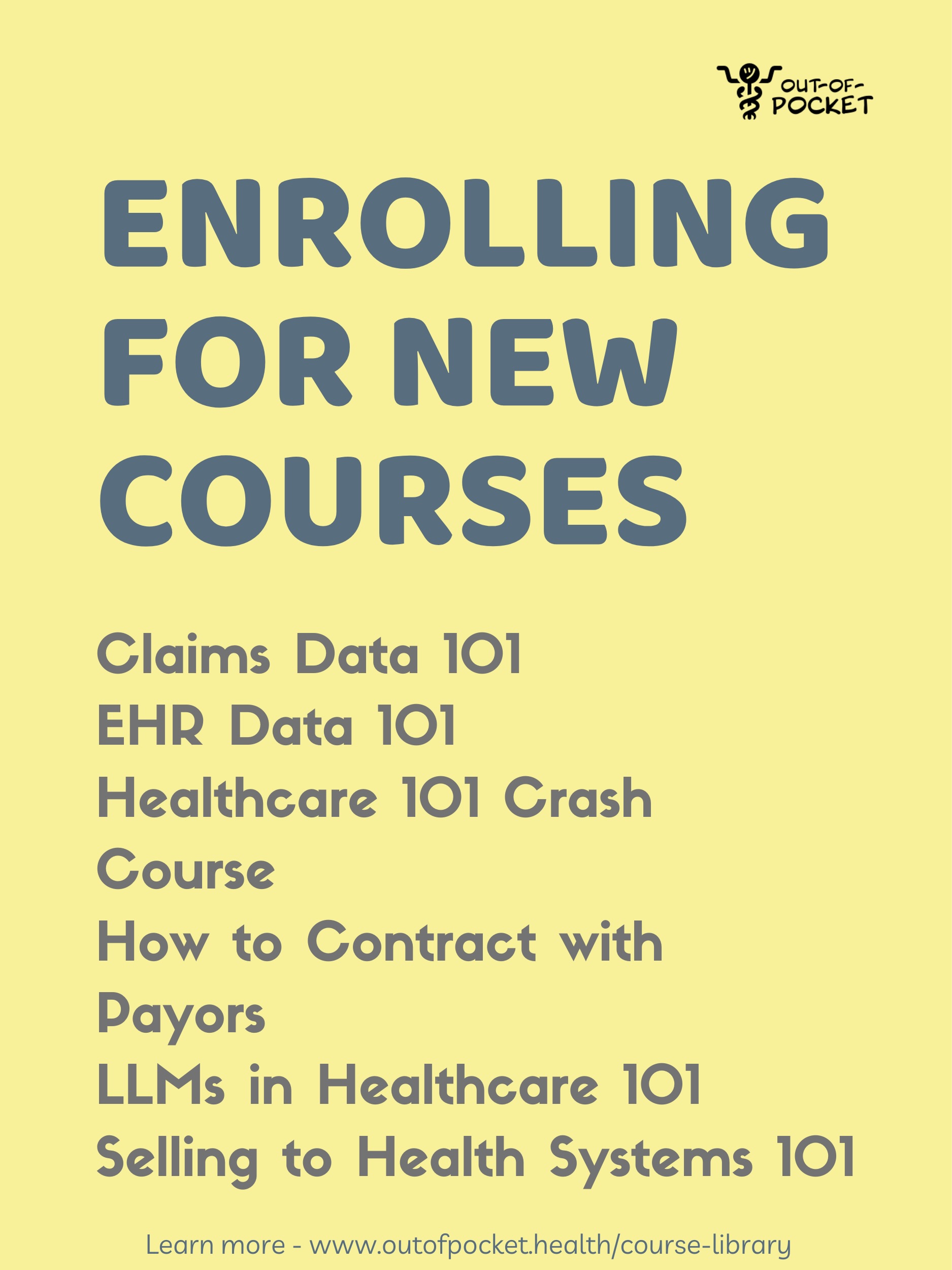
If you don’t know what value-based care is or how it works, congrats you’re qualified to post on LinkedIn about value-based care. But also I wrote a primer about it here and we’ll be talking about some aspects of it in the “How to Contract With Payers” course (starting 12/2).
I’m surprised at how consensus the idea is that the goal of US healthcare should be to move to a value-based care system. There’s an inherent belief that fee-for-service is default bad and value-based care is default good.
In my mind, value-based care simply presents a different set of tradeoffs. For example, fee-for-service is extremely easy to administer, but difficult to incentivize more cost-effectiveness into patient care. Value-based care adds cost into the care equation, but is difficult to administer and requires many more lawyers, actuaries, staff, and software that favors larger institutions.
It’s not entirely clear that one is DEFINITELY better than the other. But you can tell which one consultants like more.

I’ll write a future post that looks into different dimensions of value-based care and whether it’s working. But here’s a quick set of high level takes:
Optimistic take - While they won’t win on every metric, lots of value-based care programs have had promising results. The Maryland All-Payer model was able to keep costs controlled without quality sacrifices. The Home Health Value-Based Purchasing Model managed to keep costs low and reduce unnecessary utilization of skilled nursing and other high cost services. The Medicare Shared Savings Program has mixed results, but seems to be working in specific instances/applications (e.g. amongst physician-owned groups).
Relatedly, to succeed in many value-based care programs you need to use team-based care. Compared to fee-for-service, there’s much more flexibility in being able to use different types of labor in more appropriate places. When so much of healthcare is just helping patients navigate everyday life, being able to shift more responsibilities to peers, social workers, etc. without being constrained by the payment model feels like a win.

Value-based care is an ever evolving experiment that we’re still in the very early innings of. Fee-for-service is hundreds of years old, value-based care is realistically like 15. We learn from old experiments and change things in new models as we learn.
You can already see this in some of the newer models that CMS is putting out. AHEAD is shaped from the previous all payer models like Maryland. ACO PC Flex is an experiment within Medicare Shared Savings to see if it’ll help smaller provider groups join the program since they seem to perform well. ACO REACH is a value-based care program that was built off of several other Accountable Care Organization (ACO) programs in the past. Even methodologies like how risk adjustment gets calculated in Medicare Advantage are changing so that it’s not so easy to game the coding system just to get bonus payments.

And these are just the government programs - a lot of which inform private plans on how to structure and evaluate their own value-based care arrangements with vendors. All in all, the feedback loops on any of these programs take a while. We adjust/iterate as we learn what works and what doesn’t in each program to try and improve future ones.
Also why do ACO programs sound like a rap group? A¢O is the new A$AP mob.
Neutral take - There’s simply too much apathy and workflows built in the current healthcare system for any meaningful change. Value-based care requires a massive operational lift from anyone that’s participating in it, and the providers you most want to participate won't unless forced. The areas you’ve seen the most adoption of value-based care are places where the operational lift is low (e.g. don’t need to change what clinicians do too much) but the additional revenue is high (e.g. upcoding for higher reimbursement).
We’ll discover that certain patient populations with high preventable spend are where value-based care is particularly useful. In the Direct Contracting program, you saw most of the success and savings in high needs patients. A company like Bloom Health that focused on these patients was by far one of the top performers. For these portions of the population, we’ll double down, new provider groups will focus explicitly on those populations. More likely than not it won’t reduce overall spending, but for those patients the care will be better.

The rest of the population just sticks to good ole’ fee-for-service like usual. Value-based care will always be a small percent of healthcare dollars that largely don’t change how care is delivered.
Cynical take - Value-based care gets pushed by a lot of non-physicians because it creates a need for people like us and it feels good to say abstract things like “we help improve patient outcomes”. Eek that sounds mean as I say it; sorry, Wharton MBA grads.
More structurally, having multiple insurance types and prices means that any savings from one side will result in increased prices on a different side. Payers and providers negotiate healthcare services across all of their different plans - payers can suggest a hospital takes a value-based care related haircut in Medicare but they’ll make it up in increased fee-for-service commercial prices. That commercial insurance has the most spend in healthcare but least traction in value-based care suggests it won’t make a dent as long as we have a multi-priced system.

At its worst, value-based care encourages consolidation and makes it even harder for independent practices. Yes, there are exceptions. I feel like the Aledade people are looking up where I live as we speak.
But gathering quality metrics, buying software, hiring extra staff, getting outsourced analytics expertise, needing to pay lawyers and consultants to navigate kickback laws and contracts…this is a lot of stuff that is just infeasible for small practices. On top of that, many value-based care programs have a minimum number of patients before you can participate in the program (for example, in ACO Reach the minimum for new entrants is 4,000 Medicare patients). This op-ed in JAMA goes into many more of these details.
Interlude - Healthcare 101 enrollment ends this week
Healthcare 101 starts next week, enrollment for it ends this week. It’s the fastest way to learn how US healthcare works, taught by yours truly. You can sign up for it here.
We go through all the major stakeholders, how money flows through the system, basic laws and regulations to know, and lots of the buzzwords like what actually is value-based care and practical challenges with it.
It’s the best place to throw down your not-hard-earned learning stipend, and you can email me back about group discounts (3+ people) at nikhil@outofpocket.health.

Alternatives?
Value-based care gets a lot of airtime in the conference circuit and social media. When CMS announces a new model it’s like the Superbowl for people who know what “Wakely” is. But maybe it gets too much attention vs. other potential attempts to improve healthcare.
I know many of you will send your takes about specific parts of value-based care programs, so I thought I’d float some other ideas that I think we should focus more on.
What about consumer-driven value-based care? Today the idea of value is decided from the top down - governments and insurers picking metrics that count as quality. But my hunch is that these sentiments of value don’t always line up with what consumers think is valuable. CMS cares about “% of patients readmitted”, I care about “not throwing out my back when ‘Wobble’ comes on at a wedding”. What if there were more experiments on “bottoms-up” value-based care?
For example, Taro (disclosure: investor) is a new health insurance carrier that wraps around Direct Primary Care (DPC). DPC doctors take a monthly subscription fee and cover a menu of services underneath that fee.
Inherently those direct primary care doctors need to offer “value” to patients otherwise they won’t keep paying that fee, and the arrangement is pseudo “capitated” in the form of a monthly fee. But each physician-patient relationship will have a different idea of value, some patients might look for doc with 24/7 texting while another will want them to have experience managing their condition. Taro is betting that by having an actually consistent relationship with their primary care physician based on whatever the patient finds valuable, their health will be better managed long-term.

In essence this is still an experiment in “value-based care”, we just don’t really call it that. But it has a few unique quirks:
- Smaller practices can participate in something like this.
- The focus is on what patients want, and that can have a wider variety of options at the outpatient level.
- It can still use a fee-for-service chassis for non-primary care issues.
- You don’t need a PhD in self-loathing to understand how it works
The obvious limitation here is that it focuses on primary care when the bulk of spend is in specialist visits and hospital stays. Plus it’s constrained by the number of direct primary care docs and patients they can see. But I think it’s still worth experimenting with other models, and I think it can work in outpatient specialist care as well.
Bounties for new cures, drugs, and more - Should we direct value-based care dollars towards developing drugs, medical devices, etc. instead? Would that be a better ROI? Obviously it’s not so mutually exclusive, but this is a thought experiment.
GLP-1s are expensive today. In the next few years it will likely compete down in price and we’ll also get results on savings from people that have been on them for a few years. My prediction is that GLP-1s will end up saving more money in 10 years than value-based care will, and if I’m wrong I’ll probably be in a prepper bunker anyway where you can’t find me.
When you look at drug pipelines, upcoming medical devices, etc., they focus on areas that are lucrative to get reimbursed but not 100% aligned with societal value.

End Stage Renal Disease represents more than 6% of Medicare alone and privately insured patients can be more than $238K a year after starting dialysis. Why aren’t there hundreds of companies attempting cures? Xenotransplantation of pig kidneys is promising, ARPA-H is funding moonshot bioprinting companies to 3D print organs, but it feels like there should be way more attempts to fix it. Where are the weirdos trying to make portable dialysis machines? Where is the Operation Warp Speed equivalent of fixing the kidney transplant list?
Clearly there’s a commercial market here, the issue seems to be finding plausible ideas that might even work and funding a portfolio of attempts. Should we just take all the attention and dollars from kidney focused value-based care programs and fund inkling moonshot companies instead? Should we create incentives for payers themselves to fund these kinds of moonshots (e.g. make grants to companies pursuing cures count as a medical expense for Medical Loss Ratio calculations)?
Obviously, this is easier said than done, but maybe we should have more moonshot programs in these areas vs. just cancer. At the very least, payers should care more about solving these problems than just paying the bill when it comes.
Giving patients money directly - A big part of value-based care is the idea that the healthcare system should help patients outside of the four walls of the hospital. This is increasingly trending towards helping with non-healthcare needs like food, housing, etc.
I think we need to ask whether a dollar filtered through the inefficiencies of the healthcare system with every middle entity taking a 10% cut will yield more positive health results than just giving the patient a dollar directly. I would argue that SNAP benefits to help buy food is a better use of a dollar spent to help healthcare than one that goes through a total cost of care program that includes covering food.
It’s hard to definitively show social safety net programs alone improve health alone because they happen over such a long period of time. There are some papers that show SNAP reduces obesity/heart disease or improves self-reported health outcomes for seniors. Two papers on universal basic income (here and here) were published this year: both found an increase in utilization of outpatient services, but one that studied long-term health found that the positive health effects subsided after the first year.

But we have a weird obsession with proving the ROI of programs in value-based care and adding layers of management and infrastructure to track that vs. just admitting intuitively reducing food insecurity or alleviating poverty through massive programs like the Earned Income Tax Credit/Child Tax Credit will probably improve health.
The reality is that it’s politically easier to funnel money to groceries through the lens of reducing healthcare spend than on “welfare” programs, which is sort of sad. So we set-up elaborate programs in the healthcare system to track everything closely.
North Carolina has a “Healthy Opportunities” program to allow Managed Medicaid Organizations to pay for a set of social services they think will help health outcomes. Managed Medicaid is a form of value-based care, and in theory the aspirational goal for value-based care organizations is to help with more upstream issues like food and housing. It’s a program that has $650M earmarked for it.
It took three years and $27M to set up the infrastructure that would allow Medicaid programs to pay for social services and food. $100M is earmarked to help community organizations set up the infrastructure to be able to send invoices to Medicaid, judge member eligibility, etc.
After 3 years…10 people had received food!!! I have personally fed more people in one evening. Even after 5 years, <$10M per year has actually been reimbursed which still seems low. It’s no small feat to pull this off, I don’t want to trivialize the effort. But is a dollar going through the value-based care pachinko machine below better than just giving it straight to the patient?

Parting thoughts
The purpose of this post isn’t to say value-based care is bad. We’re not going to be able to have that discussion in one newsletter. Plus I already wrote that draft but it got torn to shreds from my feedback posse.
This post is meant to widen the lens of ways we talk about “value” in a healthcare context; maybe it doesn’t need to be a new CMS model with a quirky acronym that spells out its goal.
I just think we should be trying experiments that make healthcare simpler for patients and physicians, value-based care adds a ton of complexity. Like in order to take part in ACO REACH, your doctor needs to understand the equation below.

This post is also a chance to hear your thoughts on value-based care and whether it’s a goal worth pursuing. I’m not on the frontlines directly working on this problem like some of you are, so I’d love to encourage a conversation about this.
Let me know how your thoughts on value-based care have changed or if there are specific slices of healthcare you think it definitely works or definitely doesn’t. I’ll include my favorite answers in the next newsletter, especially if they include specific examples or stories.
Thinkboi out,
Nikhil aka. “A¢O NIKHIL - Navigating Integrated, Knowledge-driven Healthcare for Improved Lives” CMS you can hire me to do your names.
Thanks to Ankit Patel, Ajay Haryani, and Manas Kaushik for reading drafts of this
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
--
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.