Time Toxicity in Healthcare - A Real-World Example
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Network Effects: Interoperability 101
.gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
I’d like to highlight more patient journeys
by Nikhil Krishnan and Laura Stratte
I think it’s easy for me to sit in my Eames chair and wax poetic from afar about issues in healthcare. But getting perspectives from the frontlines can help us all understand the practical pain points patients and physicians feel, so I’m trying to do a better job of incorporating those perspectives.
Today, I’m publishing a post from Laura Stratte. Laura and I did an interview a few years ago about what being a cancer survivor and cancer care navigator looks like. The role of a cancer navigator is really fascinating - Laura and I talked about exactly what that entails a few years ago which includes all of the logistics associated with getting to appointments, navigating insurance, coordinating schedules of multiple parts of the hospital, etc. It also makes you acutely aware of all the “tasks” patients have to do when they’re a cancer patient.
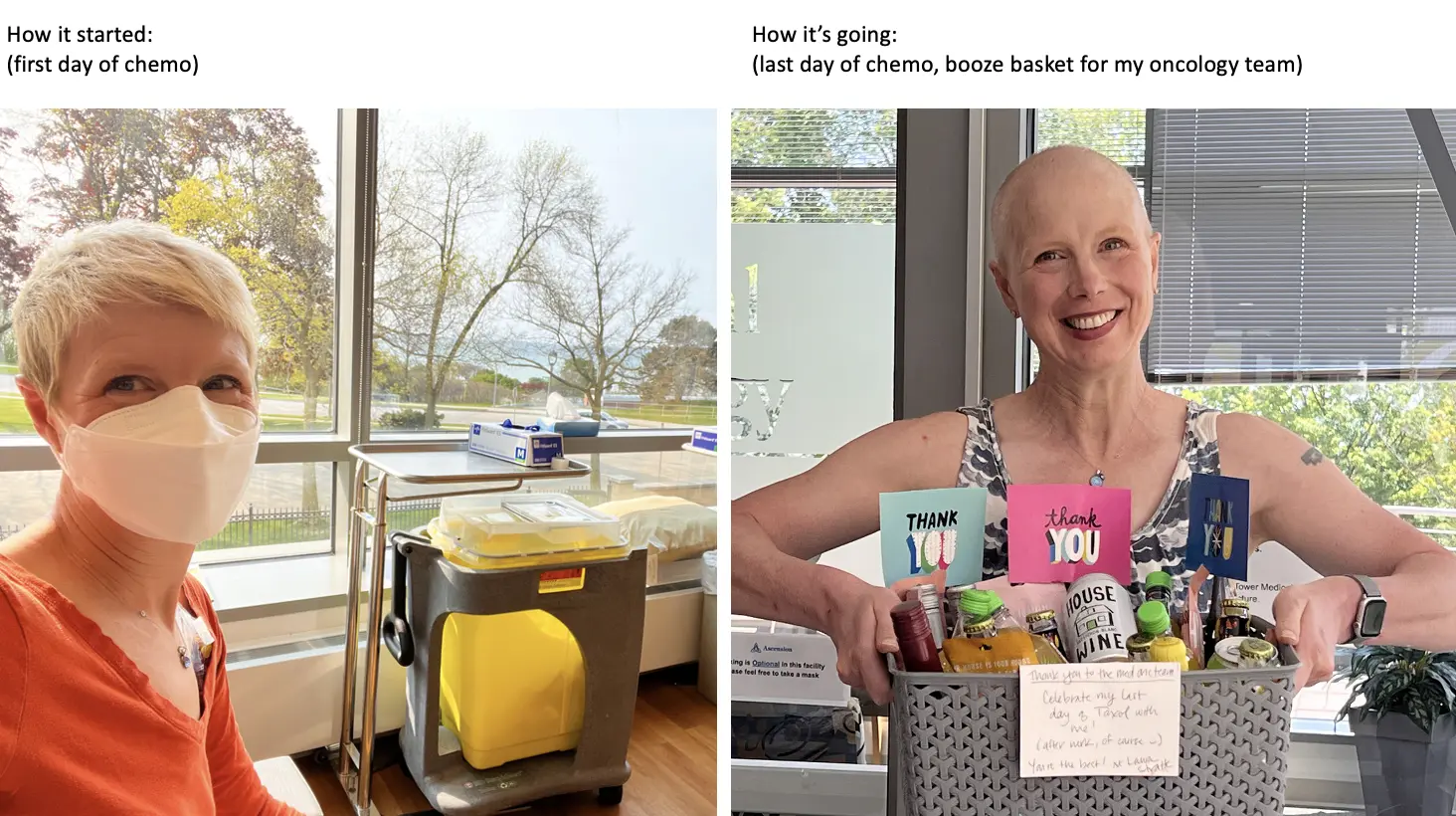
Unfortunately, Laura discovered her cancer was back recently. But Laura is a trooper; she’s absolutely suplexing the cancer. And this time around, she ran an interesting experiment where she tracked all the time she spent doing stuff for her treatment.

One of the things we talk about in healthcare is how inconvenient it can be for patients to go to the doctor, find a time that works in the middle of the day, spend time juggling insurance, etc. But Laura explains exactly how real that cost is in her personal life.
For anyone interested in the cancer journey and inconveniences sick patients face, you should read Laura’s time tracking post below. A little levity and memes added from me, the ultimate test has always been seeing if we can make cancer funny.
—
Unfortunately, the cancer is back
On Saturday, April 1, somewhat delirious from jet lag after a 28+ hour travel day home from a trip to Portugal with my daughter, I found a lump on my right breast - my cancer breast. I was a couple of months shy of the 15-year anniversary of the diagnosis of my 2008 breast cancer. Maybe my lumps are a leading indicator of recessions?
This lump was pea-sized, mobile, and sat right under the skin, on top of the upper edge of my subpectoral implant. It was visible to the naked eye and I wondered how long it could have possibly been there. Clearly I’m not doing enough mirror affirmations or I would have noticed.
After my first diagnosis, like many cancer survivors, I became hypersensitive to every ache, pain, or sensation I felt. Imagine you got the WebMD “oh i think it might be cancer” pang but all the time. Over the years, that sensitivity wore off, and as I worked as a breast cancer nurse navigator, I learned to follow a two-week rule: if I noticed something weird, I would wait two weeks. If it was still there, I’d call the doctor.
But on that April Fool’s Day morning, the day I discovered the lump, I reconsidered my rule, and decided to go another route. I asked myself “What would I tell a patient to do in this situation?” And the answer was easy and absolute: Don’t wait. Get it checked out now.
On Monday morning, I called my doctor and my former colleague who was still navigating patients at the cancer center where I was treated in 2008, and where I worked until 2020. She went into coordination mode, as navigators do. She looked at the breast imaging schedule and squeezed me in for an ultrasound over lunchtime on that Wednesday, April 5 which was only doable because the cafeteria was serving dry grilled chicken once again. The radiologist thought it was nothing but couldn’t be sure, so to be on the safe side he recommended a biopsy over observation. Sure maybe they had some RVU targets to hit, but I wasn’t in the mood to lecture about fee-for-service incentives right then.
I took the next available biopsy slot which was early the following morning (lucky!), and my pathology results came back the next afternoon: it was cancer, again (unlucky!). My other nurse navigator, who's also a former colleague and friend, called to give me the news. It took my breath away.
On the following Monday, April 10, as I pulled myself together and as treatment coordination was getting into full swing, I saw this STAT article about time toxicity, or how much time cancer treatment and all that it can involve (care coordination, dealing with side effects, sitting in the waiting room, etc.) can take. In cancer care, we’ve been talking about the concept of financial toxicity for years. We know that cancer just doesn’t affect our physical and mental health. But I had never considered the idea of time toxicity, which was odd because personally and professionally, I knew full well how much time a serious medical condition like cancer could take.
I’m a big healthcare nerd and I like to keep organized. Since 2004, I’ve been tracking the healthcare utilization of me and my family on a spreadsheet, one tab per year, with extra tabs for vision and dental. Yes I did well in group projects in school. Every doctor visit, immunization, prescription, wait room music genre, copay, co-insurance, etc is noted.

So when I read that Stat article and this 2022 article from the Journal of Clinical Oncology, I decided to add one more element to my table: time. This case study outlines my experience, and what I’ve learned.
How and what I tracked
Taking a cue from the 2022 paper, I set up some tracking parameters. I would start tracking retroactively from April 1, when I first noticed the lump in my breast, and track through September 20, the end of my active treatment (see below).
I would track all of my healthcare touchpoints: visits, treatments, trips to the pharmacy, imaging, procedures, the time I spent going over bills (on my own and with my insurance company or hospital billing), and any care coordination activities, like talking to my navigator or calling the clinic to make appointments. For any touchpoint that required I leave the house, I would track total door-to-door time.
As I explain in more detail below, I didn’t track recovery time other than the day after my surgery, time when I had to skip out on regular activities due to fatigue or side effects, or household / family care coordination.
Treatment overview
- My initial workup was a little over 3 weeks.
- After that, my treatment started with an outpatient surgical excision
- It was followed by 12 weeks of weekly chemotherapy paired with a targeted therapy administered every 3 weeks
- After the 12 week of chemo, radiation therapy followed for 5 weeks, with treatments daily Monday - Friday.
- Although I’ll continue targeted therapy for a full 17 cycles and will start on 5-10 years of hormone therapy, for the purposes of this study, I consider the last day of active treatment to be the last day of radiation, which coincided with my 7th cycle of targeted therapy.
My workup consisted of a breast ultrasound> biopsy > breast MRI > another breast ultrasound > another biopsy > PET scan > echo > genetic counseling and testing > and pelvic ultrasound because of an MRI finding. After treatment started, I had another echo and follow up pelvic ultrasound.
[For the oncology nerds out there: It’s a right breast mucinous carcinoma, ER+/PR+/Her2neu+ (weird, right?), Stage 1, T1bN0M0.]
Treatment included surgical excision with sentinel node biopsy + port placement (April 27) > weekly Taxol x 12 (May 17 - August 2) and Herceptin every 3 weeks (May 17 through end of April 2024) > 5 weeks of whole breast radiation (August 16 - September 20). I started endocrine therapy on November 1, which I’ll continue for 5-10 years.
What I Spent Time On As A Patient
I looked at two main measures: the time I spent on healthcare touchpoints in hours and minutes, and the number of days when I had a healthcare touchpoint. I'll refer to these as healthcare days. For reference, there are 173 total days between April 1 and September 20, and of those, 121 were work days excluding weekends and Memorial Day, July 4th and Labor Day.
With these in mind, there are 4 primary takeaways.
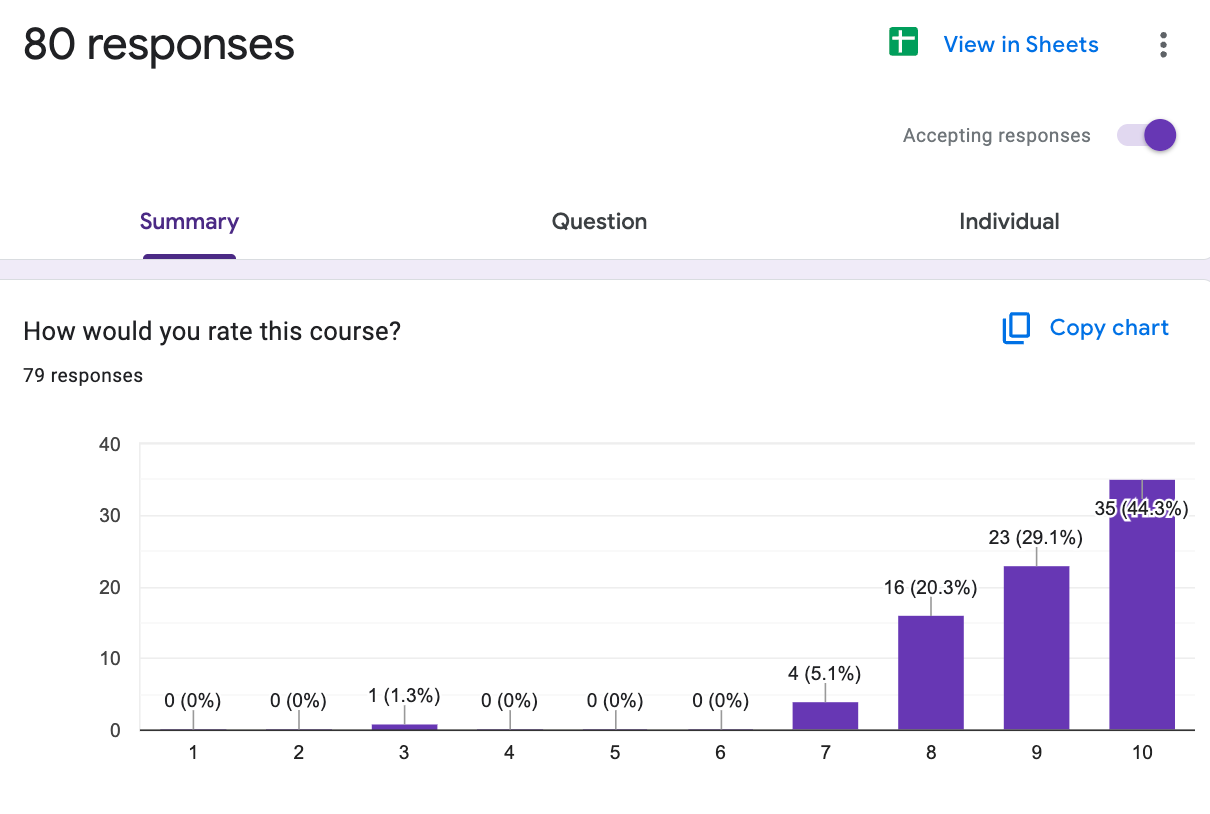
1. I spent 129.5 hours on healthcare touchpoints and had a touchpoint on almost 40% of total days, or 55% (!) of work days.
By month, the hours I spent ranged from a low of 15.75 hours in September, to a high of 26 hours in April. These same months were my top for the number of healthcare days - I had healthcare days in just over half of April and almost ⅔ of September. Now I get that whole Green Day song.



Essentially, when you have cancer and are going through treatment, it’s almost impossible to separate yourself from it. It’s emotionally everpresent, and it’s practically there too. Cancer becomes a part-time job, a chore, a regular, frequent unpleasant thing you have to do. Its presence is always felt, and the amount of time spent only amplifies this.
2. I had to take off 13% of my work days during treatment, and had a visit to a healthcare facility at least one day per week for every week during the 5.5 months I tracked.
I spent the equivalent of 16.2 work days (assuming 8 working hours per day) on cancer.
In practical terms, what does this mean? As I stated above, it means that during the entirety of this 5.5 month period, I never once had a week during which my work schedule wasn’t reduced. My productivity was absolutely affected. But I’m lucky to work for a company that’s incredibly supportive and flexible, in a role where I could take off for an hour in the middle of the afternoon for an appointment if needed, with coworkers who were always ready and willing to fill in for me when needed.

Is every cancer patient so fortunate as they go through treatment? Definitely not. As a nurse navigator, I witnessed firsthand the stress experienced and sacrifices made as patients tried to make their treatment work with their jobs. Adding on shifts on their non-treatment days, missing appointments because they couldn’t get someone to cover their shift, adding on a part-time job to make up for lost wages.
To make matters worse, not everyone is eligible for medical leave, and even with those protections, I can tell you that accessing medical leave benefits can be tough and add on a ton of time. Some employers ask for ridiculous details of treatment plans that would inevitably change, requiring forms to be filled out multiple times. This meant the patient had to chase down a member of his or her care team and have someone fill the forms out again and again.
3. Most of my time spent (69%) was for treatment, as expected - but I’ve spent WAY too much time on billing issues.
Chemotherapy was the most time intensive, taking almost half of my time. Radiation was next, coming in at almost a quarter. To put this in practical terms, during my 12 weeks of chemo, I took about ½ day off per week. During 5 weeks of radiation, it was ~1 hour per day. But at least these treatments were planned well in advance, which meant that I could plan ahead, which made life easier for everyone involved.

And yet somehow going through chemotherapy and dealing with cancer was less painful than dealing with the billing department. I’m both literally and figuratively ripping my hair out.
I’ve spent 5% (about 6 hours*) of my total time to date on dealing with billing, which is 3x as much as I spent on the phone coordinating care. And there is no doubt this number will increase significantly because most of my bills for treatment haven't come through yet. (In fact, at the time of this edit - about 2 months after the end of treatment - I’ve spent at least 3 more hours on the phone with insurance and the billing department.)
Here are a few of the issues I had to work through:
- Figuring out why the claims for targeted therapy treatments were denied. My insurance company incorrectly told my hospital that a prior authorization wasn’t needed for my targeted therapy, which should have immediately made me suspicious. Now I had to figure out what was being done to remedy that situation - did I need to do anything? I talked to folks and they seem to be figuring it out but at this point, I have no idea of the status. I guess I’ll just wait and see when I get billed?
- Managing discrepancies in billing information across various platforms. I would see that I owe $X in MyChart, but that included what was still being processed by insurance - so I could see a bill for several thousand dollars (which, you know, is not fun to see) but in the end I would owe just a fraction of that. I understand how insurance works, but why show me what I might not have to pay? Then, every few weeks a PDF bill appeared in MyChart, I would get notified, but when I went to the bill pay platform, I couldn't pay it because it said I had a $0 balance. There is a delay in there so I would have to keep checking to see when I could actually pay. A note to hospital billing departments: Don’t tell me I owe something before I actually owe it, and don’t tell me without the ability to pay it.


4. The pre- and post-diagnosis workup is a killer (no pun intended).
A work-up is essentially figuring out what’s going on - it can involve labs, imaging, biopsies, etc. to get a diagnosis. After that diagnosis there are usually more scans, imaging, biopsies, etc. to learn as many details as you can about the particulars and the extent of the disease so a treatment plan can be developed.
From April 3 - 20 during my pre- and post-diagnosis workup, I had ~18 hours of healthcare time over the span of 14 work days. Much of this was imaging and biopsies which accounted for 9% of my total time but 70% of this workup time. And biopsies. These types of visits can be a bear to schedule, and you essentially take whatever appointment you can get - you really don’t have many options - and hopefully your life can work around that. It’s really tough to work and keep life plans when appointments are basically them calling and hoping you do 90 on the freeway because a slot just opened in 20 minutes “if you can make it”.
I was on the other side of this when I worked as a nurse navigator. I know what scheduling in hospitals and clinics is like and why it is the way it is, but we’ve got to figure out a way to make this better.
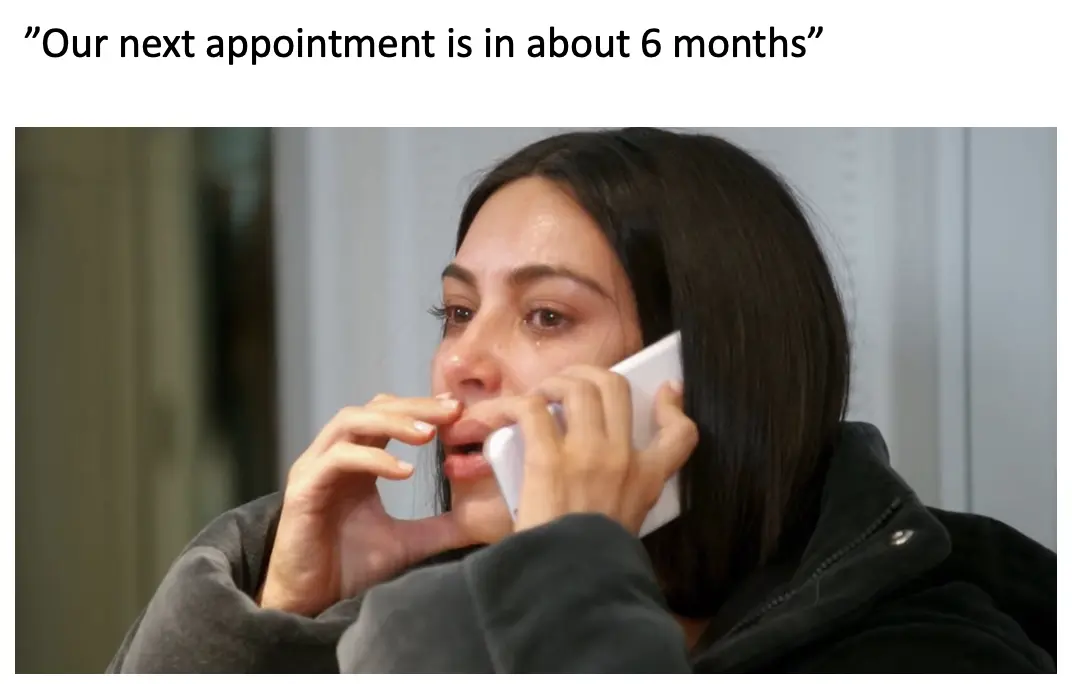
Waiting is one of the worst parts of the work-up phase. You schedule every test or scan, wait for it to happen, then wait for results, then wait for the inevitable follow-up test or scan, and the process repeats itself over and over. You’re constantly checking your phone or MyChart for messages. The kids are scrolling through Tik Tok and I’m over here addicted to MyChart, it’s embarrassing.
The anxiety that comes with the uncertainty of this phase is heavy and sticky - it’s so in your face it can be hard to focus and even function at times. I so badly wanted to press fast forward to the point where we knew what we were dealing with so we could make a plan moving forward - but all I could do is sit, try and distract myself, and wait it out. This is another factor in the time toxicity of cancer that is almost impossible to measure, but it’s there.
Discussion (none of the real journals accepted this so I’m stuck with Out-of-Pocket, humor me)
When I was at the cancer center on my last day of treatment, I joked with my care team, saying that I was ready to quit the part-time job that is cancer treatment. When I look at these numbers, I find that I really wasn’t joking. Cancer treatment is a part-time job, just like being a newsletter writer.
BUT - when I look at things objectively, compared to some of the patients I’ve worked with in the past and others I’ve known who have gone through, I know I’ve had it easy:
- Almost all of my care was done at a center that was an easy 15 minute drive from my house, and the small amount of care that wasn’t done there was done at a center 20 minutes away.
- I have a car, so I didn’t need to rely on public transportation.
- Parking was easy and close. I could hop in my car that was sitting in the driveway, and once at the cancer center, pull into one of the many open spots and walk from my car to the front door of the clinic in 1 minute. Some medical centers have huge campuses with giant parking structures, which could mean a 10 minute walk coming and going. Side note, some healthcare campuses make 80% of their operating revenue from hospital parking.
- The cancer center where I was treated was compact and everything was in the same building. My surgeon’s office was on the third floor, medical oncology was on the first, and radiation oncology was in the basement. The hospital where I had most of my imaging was across the street. I can’t stress how much this made everything more convenient. This meant that I could easily piggyback appointments, like one day when I went checked in at med onc and had my vitals and labs taken, ran downstairs for my radiation treatment, and ran back up to get my Herceptin.
- I had amazing navigators who did the bulk of scheduling for me, especially in the beginning.
- For chemo, my labs, doctor’s visit, and chemo administration could happen on the same day, and the lab was speedy, it almost always took under 30 minutes for lab results to come through. At some clinics, these functions can be spread out over two days: first, you go in to see the doctor and have your labs drawn, and then you come back the next day for the actual infusion. This is double the travel time, and turns what could be one healthcare day into two.
- I fared well during my treatment and didn’t have to deal with any adverse events that required a special visit, nor did I have to bail out of many activities because of side effects. My surgery was easy, my chemo regimen was relatively lightweight as far as poisoning entire parts of my body goes. Although I had a rather severe skin reaction that had barely started by the tail end of radiation, it didn’t really affect my day to day until after this time study was over. Overall, my most bothersome side effect was fatigue, but that was relatively minimal and I was able to handle it well with prioritizing sleep and exercise, and managing activity.

Without all of these conveniences, I have no doubt that the time I spent would have at least doubled.
I also need to consider my social situation. I chose not to track time spent on the secondary effects of treatment like coordinating childcare, planning meals, rearranging any home or work schedules because I didn’t experience many of those secondary effects. This time around I had a flexible employer and my caregiving duties were light, which is unfortunately not the situation for most patients.
The first time I had cancer my kids were 2 and 5 and it was a completely different experience. I spent a ton of time making arrangements for rides, activities, meals, shopping, etc. It took longer to schedule treatment because of the back and forth needed to make sure I could find childcare coverage for the available appointment slots. And day-to-day activities took more effort too. I had to be careful managing activity so I wouldn’t crash, and needed to find things for my kids to do that summer to give me some rest time, which was tough because by then all camps were full.
And consider the time my husband spent on taking over the duties I usually did, or the time my family and friends spent helping me. Tending to these sort of life coordination duties takes time, and that time adds up, and it can be significant. That’s all part of the time toxicity.
Laura’s Conclusion
As I reflect back on my recent cancer experience, I see everything, outside of the diagnosis itself, as a best case scenario. Despite the time it took, despite the frequency of my treatments, it really wasn’t that bad. (Well, I take that back - dealing with billing and insurance issues is always, always bad).
But then I think back to patients I worked with when I was a navigator, and stories from other patients I’ve met along the way, and I’m ashamed to say that I never thought about how much time cancer takes until now. And I was part of the system. Even in ideal circumstances, cancer is intrusive, all-consuming, and the toxicities we experience penetrate every aspect of our lives. But the good news is that the cancer care community is recognizing more and more of these under-the-radar side effects, starting to talk about it, which is the first step in actually addressing them.
As someone who’s had cancer, I believe it’s my obligation to make things a little bit better for the next person. I’m hoping sharing my story can do that.
Thinksquad out,
Laura and Nikhil
Twitter: @nikillinit
Other posts: outofpocket.health/posts
--
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!!
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
Selling to Health Systems (starts 10/6) - Hopefully this post explained the perils of selling point solutions to hospitals. We’ll teach you how to sell to hospitals the right way.
EHR Data 101 (starts 10/14) - Hands on, practical introduction to working with data from electronic health record (EHR) systems, analyzing it, speaking caringly to it, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →Our Healthcare 101 Learning Summit is in NY 1/29 - 1/30. If you or your team needs to get up to speed on healthcare quickly, you should come to this. We'll teach you everything you need to know about the different players in healthcare, how they make money, rules they need to abide by, etc.
Sign up closes on 1/21!!!
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.

Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.