What Do Hospitals Care About?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Network Effects: Interoperability 101
.gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
The Real-World of Hospital Orgs
Last time, Ben Chao and I talked about how hospitals can be organized. Which ones have emergency departments and not, what are some of the designations they can receive, and the strange relationships between hospitals and “hospital-affiliated groups”. You can see the full post here as a refresher.
Most of you had the same question: “who fucking cares?”
And so we decided we’ll double down on this topic. Today we’ll talk about some of the things hospitals prioritize and how their organization structure might change as a result, including using a real example of St. Charles Health System.
What Are Hospital Priorities?
Hospitals create internal strategic plans and invest accordingly in their operations. Decisions on where to invest bandwidth and capital are driven by many things. But today we’re going to focus on operational urgency, strategic positioning, return on investment, community need, and balancing the public perception that they have no money but also have the best, high quality facilities for care.
Let’s go through each.
Hospital Priority 1: Operational urgency
Where do we have the most critical operational deficiencies? Do we have a piece of major equipment (i.e. an MRI machine) that is past its manufacturer recommended useful life and is now showing signs of breakdown? Tell the MRI machine “same bro”, and buy a new one.
Do we have throughput challenges that impact our financial performance? A common thread here is when process challenges extend a patient’s length of stay (LOS). Fee-for-service hospitals often get paid a fixed amount based on what the payer (especially Medicare) believes the length of stay should be, so staying longer than that means the hospital will lose money if they discharge the patient too late.

The choke point could be anywhere - in the emergency department from the moment they’re triaged to admission to an inpatient unit, in the time it takes to discharge from the hospital to home, in getting timely ancillary orders done, etc. Hospitals will increase their staffing or patient-bed ratios or try to expand capacity wherever the backlog is.
In some cases, facility constraints take hold and it is literally impossible to expand the emergency department or add another unit of inpatient beds, be it due to construction or regulatory reasons.
Performance on a key quality metric that drives patient mortality or other bad outcomes. An example could be door-to-balloon time (D2B) for patients experiencing a ST-elevation myocardial infarction (STEMI), a type of heart attack with blockage of a coronary artery. Door-to-balloon time measures the duration from when a patient arrives at the hospital to when a catheter guidewire crosses the blocked artery, inflating to relieve the blockage. Longer D2B times increase the likelihood of death or damage to the heart, so a hospital may make a decision to shorten D2B times if they are consistently unacceptable.
There’s the “do the right thing” reason why they do this, but there’s also business reasons. Better doctors obviously are more attracted to places that care about these aspects, and it also lets the hospitals explain their higher quality rankings to payers/patients/employers who might want them in-network.
For example - the Leapfrog Group is a watchdog organization that conducts annual quality surveys and publishes the outcomes to consumers, payers, and benefits brokers to inform value-based purchasing and decision-making. They also collate various measures - you can look up your hospital and see how it performs on different dimensions here.

Or another example, hospitals who have subspecialty patients coming to them from across the country compete for reputation through US News' Hospital Rankings. Those rankings are based on composite scores that roll up performance across several quality and patient experience measures. Just looking at that website is giving me college admissions PTSD.
Hospitals might also diversify to complementary or substitute services in case demand overwhelms supply. We see this with urgent care as a substitute for primary care by ensuring speedy access to care while hiring more nurse practitioners or physician assistants since it’s hard to find docs. Hospitals are also increasingly offering behavioral health services because their existing primary care and emergency services aren’t equipped to support patients with these needs.

Hospital Priority 2: Strategic positioning and return on investment
It costs hospitals money to source capital and pay back the interest. Every hospital project is evaluated based on its ability to either generate more operating margin (new revenue has to more than offset the cost of the project) or reduce costs in another part of the business. Of course, this is entirely dependent on what payment world the hospital lives in - fee-for-service, capitation, or somewhere in between.
Not every project has a direct return on investment. Some can be driven by a response to community needs. For example, clinics that provide entirely uncompensated care, or a service where the business model historically hasn’t been profitable. Since most American hospitals are nonprofit organizations, they are obligated to provide a meaningful amount of uncompensated charity care and other services that benefit the community they serve. Like Superbowl ads…wait…
Sometimes, the return on investment is indirect. A hospital in a fee-for-service world might invest in more primary care services at a direct loss, but anticipate generating more referral volume back to employed specialists that will do profit-generating procedures at health system-owned facilities.

Other market forces like competition and consumer demand also play a role in justifying investment. Hospitals might evaluate metrics like drive time, local payer mix, and market share in a specific zip code/service area to decide where to place their next clinic.
Interlude - Healthcare Hackathon and Product 201
Our healthcare AI hackathon is going to be in SF May 16th - 18th. The venue is sick, we’re getting some awesome vendors for you to play around with, and the applications so far already have me excited.
If you’re interested in participating, even if you’re not 100% sure, you should apply. You’ll meet some awesome builders and get to build some cool stuff. Apply here.
Also we already have our first few sponsors locked in, so slots are going quickly. Let’s chat if you’re interested.

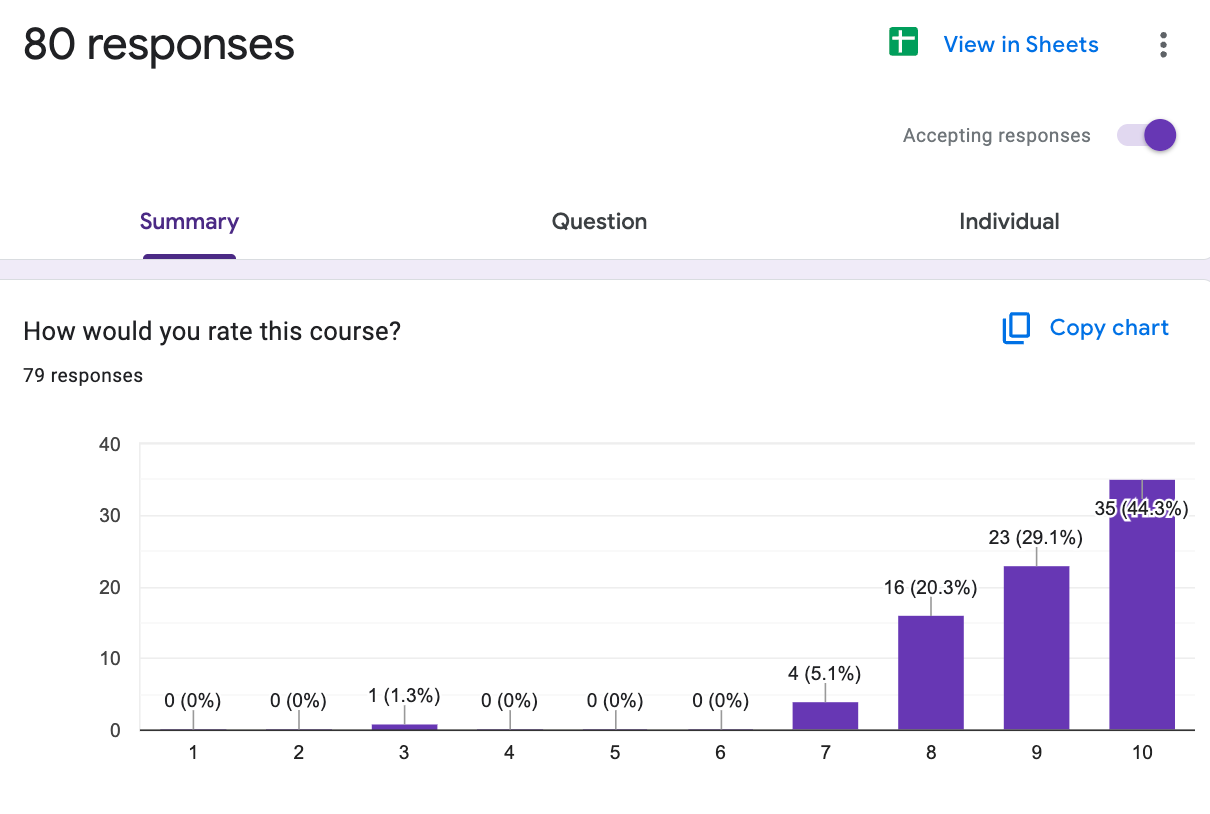
Our Healthcare Product 201 course has about 7 seats left and it’s the final time we’re running a live version of it. It starts next week and you can sign up here.
Email dhruv@outofpocket.health with questions.

Hospital Priority 3: Community Need
Most community hospitals in the US are non-profit organizations. The Affordable Care Act was enacted to ensure that nonprofit hospitals contribute to the health of their communities. Community Health Needs Assessments (CHNAs) are designed to identify the health needs of the community and guide hospitals in addressing those needs.
Nonprofit hospitals must conduct a CHNA at least once every three years. This assessment involves gathering data on community health needs, including input from community members and stakeholders.

After completing the CHNA, hospitals are required to develop and adopt an implementation strategy that outlines how they will address the identified health needs. They report the results of their CHNAs and their implementation strategies in their annual IRS Form 990. Check out Banner Health’s Form 990 here; Schedule H contains the information every non-profit hospital needs to provide that ties together their Form 990 and CHNA. Most systems with several hospitals create specific CHNAs at the individual hospital level, like Banner Health.

Compliance with the CHNA requirements is crucial for nonprofit hospitals to maintain their tax-exempt status. Failure to conduct a CHNA or to address the identified needs can result in penalties.
Some Real-World Hospital Organization Examples
Below is an example of a health system’s organizational structure. St. Charles Health System is a non-profit, four-hospital health system based in Central Oregon. We had to take some liberties from this snapshot they’ve published, but the general idea is that St. Charles operates four hospital campuses with varying levels of clinical complexity and available services, along with a few smaller medical office buildings in more rural communities.

St. Charles operates 7 primary care clinics, 3 urgent care centers, a home health/hospice agency, and its own imaging and lab services. The system made just under $1.2B in revenue in 2023 with a net operating income of $79.5M. Its hospitals are not created equal - Bend is clearly the flagship, with the most specialty services available on the hospital campus.

St Charles’s strategic plan in the 2023 annual report focuses on recovering from the pandemic by improving financial performance and resuming expansion and innovation. A $74M capital spending plan is underway to fund facility improvements and break ground on a new Cancer Center at its Redmond location, and the CHNA has shown a need in the community for more Urology and Gastroenterology providers.
The decision to invest in both the Cancer Center and these specialty services of need were likely driven by both community need and profitability. Depending on hiring plans, these investments might reflect on the org structure as a net new horizontal service line created just for cancer care with some senior reporting pathway (likely on par with the executives leading the other horizontal service lines).
It’s also likely that the cancer care service line will provide a more comprehensive set of services - medical infusions, radiation therapy, pre/post-surgical oncology care, rehab services, genetic counseling, dietitian support, clinical trials management, counseling, support groups, etc - across multiple hospitals and clinics. So now you gotta staff those up.
So that’s cancer, but St. Charles has to decide how to procure more Urology and GI bandwidth. If there aren’t any local physicians looking to affiliate or otherwise become employed, St. Charles will need to look nationally and focus physician recruitment efforts on those specialties. Now they have to think about the ROI on staff and support, which might be expensive depending on the demand to work there. Why do you think the docs in rural US have 10 bedroom mansions?
The business units from these two priorities are highlighted below in purple. Since Bend is the most sophisticated campus, future endoscopies and urologic surgeries would probably increase there at the minimum.

We talked about community health needs and ROI, but you can imagine that increasing the amount of services in one place can introduce new operational choke points downstream. If you increase a lot of endoscopies and find more cancers, what do you need to invest in to handle those chokepoints? All of these start interweaving together, in a macabre macrame of hospital departments.
Conclusion and Parting Thoughts
Hospitals are complicated beasts. They have to balance the fact that they’re a business alongside the public good that they provide. Layer on top of that a very grey area legal framework on what counts as referrals, kickbacks, etc. and you start getting some very interesting and confusing org charts. If Coase were alive today, he would faint on the spot if he saw one of these.

But understanding what hospitals are and what motivates them is key if you want to understand the American healthcare system. You won’t understand it anyway, but it’s key to knowing you don’t understand it.
In future posts, Ben and I are going to be looking at how hospitals make money. So make sure you’re signed up to get them. Or just like in general, we do fun stuff here.
Thinkboi out,
Nikhil aka. “Hospital org charts are my passion” and Ben Chao aka. “Please stop asking me to do post revisions”
P.S. We’re hosting a dinner in SF on 03/06 for ~20 healthcare ops people. if you’re VP level and above with 200+ people at your company, email danielle@outofpocket.health.
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
--
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!!
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
Selling to Health Systems (starts 10/6) - Hopefully this post explained the perils of selling point solutions to hospitals. We’ll teach you how to sell to hospitals the right way.
EHR Data 101 (starts 10/14) - Hands on, practical introduction to working with data from electronic health record (EHR) systems, analyzing it, speaking caringly to it, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →Our Healthcare 101 Learning Summit is in NY 1/29 - 1/30. If you or your team needs to get up to speed on healthcare quickly, you should come to this. We'll teach you everything you need to know about the different players in healthcare, how they make money, rules they need to abide by, etc.
Sign up closes on 1/21!!!
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.

Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







